Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (36): 5862-5867.doi: 10.3969/j.issn.2095-4344.2017.36.021
Previous Articles Next Articles
Correlation of insulin-like growth factor-1 and bone metabolism-related indexes in postmenopausal osteoporosis
Dong Mei, Wu Jian, Han Xing-mei, Jin Shu-xia
- Osteopathic Department, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China
-
Received:2017-08-25Online:2017-12-28Published:2018-01-04 -
Contact:Dong Mei, Osteopathic Department, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China -
About author:Dong Mei, M.D., Associate chief physician, Osteopathic Department, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, Inner Mongolia Autonomous Region, China -
Supported by:the Science Research Project Focus on Natural Sciences in Higher Education of Inner Mongolia Autonomous Region, No. NJSY16102; the Foundation of the Second Affiliated Hospital of Inner Mongolia Medical University, No. 2015YJJS016; the Preferred Scientific and Technological Fund for the Overseas in Inner Mongolia Autonomous Region, No. 2015025
CLC Number:
Cite this article
Dong Mei, Wu Jian, Han Xing-mei, Jin Shu-xia. Correlation of insulin-like growth factor-1 and bone metabolism-related indexes in postmenopausal osteoporosis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(36): 5862-5867.
share this article
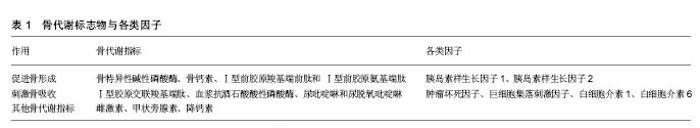
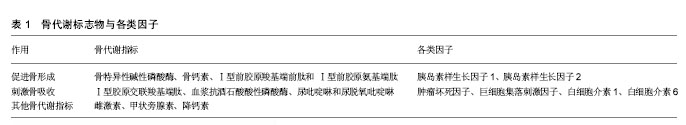
2.1 胰岛素样生长因子1与绝经后骨质疏松症 绝经后骨质疏松症,即绝经后妇女由于雌激素水平急剧下降,破坏了对骨局部因子、生长因子以及体液因子的调控,导致骨量减少及骨组织结构变化,刺激骨转换加快,骨吸收的抑制减弱,使骨脆性增多易于骨折,造成骨质丢 失[4]。女性的骨量是在骨骼的生长发育青春期完成或20岁左右增加达到峰值骨量。然后,持续稳定状态一段时间,40岁之后男性与女性的骨量随着年龄逐渐的降低,但其下降幅度随个人、种族以及性别不同。特别是,女性与雌性激素的减少与松质骨快速骨丢失主要是由于卵巢功能衰退(绝经后骨量减少,绝经骨质疏松症),之后逐渐缓慢降低。雌激素对骨代谢产生重要的影响,雌激素作用于成骨细胞和破骨细胞,使得骨吸收和骨形成同时保持稳态平衡状态从而维持骨量。雌激素对于骨骼或者其他器官均由核内受体介导表达,成骨细胞,破骨细胞以及骨细胞均具有雌激素受体样作用。对于成骨细胞,胰岛素样生长因子1可抑制细胞凋亡,刺激细胞增殖。由于这些生长因子对于骨和软骨具有同化作用,因此考虑它们可通过自分泌作用介导增加骨量。另外对于成骨细胞刺激RANKL的诱饵受体即破骨细胞分化抑制因子,从而抑制RANKL/RANK系统,抑制破骨细胞的前体细胞向破骨细胞分化。胰岛素样生长因子1是人体在生长激素刺激下产生的激素,是多种激素与细胞因子调节骨代谢复杂网络的核心因素。当脑垂体前叶分泌生长激素,在数分钟内,可促进肝细胞合成分泌胰岛素样生长因子1。胰岛素样生长因子1被细胞分泌后会与邻近细胞表面含有胰岛素样生长因子1的受体结合,它具有酪氨酸激酶活性,引起细胞内反应,促进细胞生长。研究证实,雌二醇可通过雌激素受体提高成熟成骨细胞和成骨细胞前体的胰岛素样生长因子1 mRNA水平,并呈时间和剂量依赖性[5-6]。张金山等[7]观察绝经后1-3年妇女骨密度与胰岛素样生长因子1的变化与关系,发现胰岛素样生长因子1降低可能是影响绝经后早期骨密度降低的主要危险因素。易伟莲等[8]发现绝经后骨质疏松患者胰岛素样生长因子1水平明显下降,而且胰岛素样生长因子1与骨密度、雌二醇呈显著正相关,与年龄呈显著负相关。因此,可以考虑胰岛素样生长因子1基因为雌激素发挥抗骨质疏松作用的一个重要靶基因。 2.2 胰岛素样生长因子1与骨代谢指标 骨代谢标志物迅速发展,在骨质疏松症等代谢性骨病的诊断,疗效评估和检测病情中应用日趋广泛,骨代谢的过程往往能反映成骨细胞和破骨细胞的活动及骨基质和骨矿化的变 化[9-10]。体外实验中,胰岛素样生长因子1不仅可呈剂量依赖性刺激成骨细胞前体的增殖并向成骨细胞进行分化、促进碱性磷酸酶、Ⅰ型胶原以及骨钙素等成骨标志物的表达,并且还可刺激破骨细胞的活性和数目的增加(图1及表1)。 2.2.1 胰岛素样生长因子1与骨形成指标 骨特异性碱性磷酸酶:是评价骨形成和骨转换的指标,基因定位于1号染色体。骨特异性碱性磷酸酶由成骨细胞分泌,在骨形成及矿化过程中起重要作用[9]。在成骨过程中它可水解磷酸酯,为羟磷灰石的沉积提供必需的磷酸,同时水解焦磷酸盐,解除其对骨矿盐形成的抑制作用,从而有利于成骨过程。因此,骨特异性碱性磷酸酶是成骨细胞成熟和具有活性的标志物,它被认为是最精确的骨形成标志物。郭玲等[11]在体外培养的小鼠成骨细胞中分别加入 25,50,100及200 μg/L 的胰岛素样生长因子1,结果发现胰岛素样生长因子1在此浓度范围内能显著提高成骨细胞内的碱性磷酸酶活性,并呈明显的剂量依赖效应。 骨钙素:是成骨细胞产生的骨特异性蛋白,是由依赖维生素K的γ-羧化谷氨酸蛋白即49个氨基酸组成的多肽。骨钙素是骨钙素基因转录和表达的产物,它主要参与维持骨骼正常矿化速率,并在骨骼生长以及羟磷灰石沉积时增加,是骨形成和骨转换的标志物之一[12]。胰岛素样生长因子1干预共同培养的成骨细胞和破骨细胞12 h后,明显促进成骨细胞骨钙素基因的表达并增加培养基中骨钙素蛋白含量[13]。Zhang等[14]的研究发现胰岛素联合胰岛素样生长因子1也能显著诱导基因小鼠的骨钙素启动子的活动。 Ⅰ型前胶原羧基端前肽和Ⅰ型前胶原氨基端肽:成骨细胞首先合成原胶原,在原胶原的N-端和C-端各自有一个延长肽,即Ⅰ型前胶原羧基端前肽和Ⅰ型前胶原氨基端肽蛋白酶将两端的肽切断后形成成熟的胶原。Ⅰ "
| [1] Szczuko M, Zapa?owska-Chwy? M, Drozd A, et al. Effect of IGF-I and TNF-α on intensification of steroid pathways in women with PCOS phenotypes are not identical. Enhancement of progesterone pathway in women with PCOS increases the concentration of TNF-α. Gynecol Endocrinol. 2016;16:1-4.[2] Henning PC, Scofield DE, Rarick KR, et al., “Effects of acute caloric restriction compared to caloric balance on the temporal response of the IGF-I system.” Metabolism. 2013;62(2): 179-187. [3] Gregory SM, Spiering BA, Alemany JA, et al. “Exercise-induced insulin-like growth factor I system concentrations after training in women”. Med Sci Sports Exerc. 2013;4(3): 420-428. [4] Nindl BC, Santtila M, Vaara J, et al. “Circulating IGF-I is associated with fittness and health outcomes in a population of 846 young healthy men.” Growth Horm IGF Res. 2011;21(3):124-128. [5] Khosla S, Melton LJ 3rd, Riggs BL. The unitary model for estrogen deficiency and the pathogenesis of osteoporosis: is a revision needed?. J Bone Miner Res. 2011;26(3): 441-451. [6] 燕小莉,尹曲华,康冬梅. 骨代谢指标与胰岛素样生长因子1的相关性[J]. 医学综述,2015,21(17):3097-3099.[7] 张金山,罗良平.绝经早期妇女骨密度变化及其与白细胞介素-6、胰岛素样生长因子-1和骨钙素关系的探讨[J]. 实用医学杂志,2011,27(1):54-55.[8] 易伟莲,廖德权,林柏云,等. 绝经后骨质疏松症患者性激素、细胞因子及骨代谢指标的变化及关系[J].检验医学,2012,27(4):296-298.[9] Burch J, Rice S, Yang H, et al. Systematic review of the use of bone turnover markers for monitoring the response to osteoporosis treatment: the secondary prevention of fractures, and primary prevention of fractures in high-risk groups. Health Technol Assess. 2014;18(11): 180.[10] 刘爽,杨梅. 糖尿病骨质疏松症发病机制探讨[J]. 实用糖尿病杂志. 2014, 10(6):59-60.[11] 郭玲,王敏,郝亮.胰岛素样生长因子1对小鼠成骨细胞增殖和碱性磷酸酶活性的影响[J].中国组织工程研究与临床康复, 2010,14(33):6095-6098.[12] Shearer MJ, Newman P. Recent trends in the metabolism and cell biology of vitamin K with special reference to vitamin K cycling and MK-4 biosynthesis. J Lipid Res. 2014;55(3):345-362.[13] Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. 2015. pii: S8756-3282.[14] Zhang W,Shen X,Wan C,et al. Effects of insulin and insulin-like growth factor 1 on osteoblast proliferation and differentiation: differential signalling via Akt and ERK. Cell Biochem Funct. 2012;30(4):297-302. [15] Garnero P, Sornay-Rendu E, Claustrat B, et al. Biochemical markers of bone turnover,endogenous hormones and risk of fractures in postmenopausal women: the OFELY study. J Bone Miner Res. 2000;15: 1526-1536.[16] 娄奕萌,丁晓凯,孙文学,等. 胰岛素样生长因子1在慢性肾脏病糖皮质激素性骨质疏松患者诊断中的意义[J]. 浙江医学, 2011,33(12):1763-1765. [17] Niemann I,Hannemann A,Nauck M, et al. The association between insulin-like growth factor I and bone turnover markers in the general adult population. Bone. 2013; 56(1):184-190.[18] 刘亚平,季虹,荣海钦,等. 2 型糖尿病雌性大鼠骨代谢的特点[J]. 中国骨质疏松杂志, 2008,14(1):35-38. [19] 李蔚,孙宜萍,杨建芬.脱氢表雄酮硫酸酯治疗老年男性骨质疏松症120例[J]. 中国组织工程研究与临床康复,2008,12(7):1360-1362. [20] Babatunde OO, Forsyth JJ, Gidlow CJ, et al. A meta-analysis of brief high-impact exercises for enhancing bone health in premenopausal women. Osteoporosis Int. 2012;23(1):109-119.[21] Elbornsson M, Götherström G, Bosæus I, et al. Fifteen years of GH replacement increases bone mineral density in hypopituitary patients with adult-onset GH deficiency. Eur J Endocrinol. 2012;166(5):787-795. [22] Wu Y, Sun H, Basta-Pljakic J, et al. Serum insulin-like growth factor 1 is insufficient to restore skeletal size in the total absence of the growth hormone receptor. J Bone Miner Res. 2013;28(7): 1575-1586. [23] Elis S,Courtland HW,Wu Y, et al. Elevated serum insulin-like growth factor 1 levels synergize PTH action on the skeleton only when the tissue insulin-like growth factor 1 axis is intact. J Bone Miner Res. 2010; 25(9):2051-2058 [24] Philippou A,Armakolas A,Koutsilieris M. Evidence for the Possible Biological Significance of the insulin-like growth factor 1 Gene Alternative Splicing in Prostate. Cancer.Front Endocrinol. 2013;4:31. [25] Kesavan C,Wergedal JE, Lau KH, et al. Conditional disruption of IGF-I gene in type1α collagen-expressing cells shows an essential role of IGF-I in skeletal anabolic response to loading. Am J Physiol Endocrinol Metab. 2011;301(6):E1191-1197.[26] Mormando M, Nasto LA,Bianchi A,et al. GH receptor is isoforms and skeletal fragility in acromegaly. EurJ Endocrinol. 2014;171(2):237-245.[27] Kamenicky P, Mazziotti G, Lombes M, et al. Growth hormone, insulin-like growth factor-1, and the kidney: path physiological and clinical implications. Endocr Rev. 2014;35(2):234-281. [28] Tritos NA, Klibanski A. Effects of Growth Hormone on Bone. Prog Mol Biol Transl Sci. 2016;138:193-211.[29] Appelman-Dijkstra NM, Claessen KM, Hamdy NA, et al. Effects of up to 15 years of recombinant human GH (rhGH) replacement on bone metabolism in adults with growth hormone deficiency (GHD): the Leiden Cohort Study. Clin Endocrinol (Oxford). 2014;81(5):727-735.[30] Barake M, Klibanski A, Tritos NA. Effects of recombinant human growth hormone therapy on bone mineral density in adults with growth hormone deficiency: a meta- analysis. J Clin Endocrinal Metab. 2014;99(3):852-860.[31] Crane JL, Cao X. Function of matrix insulin-like growth factor 1 in coupling bone resorption and formation. J Mol Med(Berlin). 2014;92(2):107-115.[32] Wei M, Zheng SZ, Lu Y, et al. Herbal formula menoprogen alters insulin-like growth factor-1 and insulin-like growth factor binding protein-1 levels in the serum and ovaries of an aged female rat model of menopause. Menopause. 2015;22(10):1125-1133. [33] Cavalier E, Souberbielle JC, Gadisseur R, et al. Inter-method variability in bone alkaline phosphatase measurement: clinical impact on the management of dialysis patients. Clin Biochem. 2014;47(13-14): 1227-1230.[34] Molinelli A, Bonsignore A, Cicconi M, et al. insulin-like growth factor 1 abuse in sport: clinical and medico-legal aspects. J Sports Med Phys Fitness. 2010;50(4):530-535.[35] Sun HB, Chen JC. Prevention of bone loss by injection of insulin-like growth factor-1 after sciatic neurectomy in rats. Chin J Traumatol. 2013;16(3):158-162.[36] Tritos NA, Biller BM. Growth hormone and bone. Curr op in Endocrinol Diab Obes. 2009;16(6):415-422. |
| [1] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhou Qian, Zhang Qiang, Chen Qiu. Human salivary components and osteoporosis/osteopenia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1439-1444. |
| [2] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [3] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [4] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [5] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [6] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [7] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [8] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [9] | Peng Kun. Improvement of the treatment effect of osteoporotic fractures: research status and strategy analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 980-984. |
| [10] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [11] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [12] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [13] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [14] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [15] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||

