Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (36): 5847-5854.doi: 10.3969/j.issn.2095-4344.2017.36.019
Previous Articles Next Articles
Sclerostin: a new hope for the treatment of osteoporosis
Zhang Shu-dong1, Zhu Meng-hai1, Li Shi-fei1, Yao Qi1, 2
- 1首都医科大学附属北京世纪坛医院,北京市 100038;2解放军总医院,北京市 100853
-
Received:2017-08-07Online:2017-12-28Published:2018-01-04 -
Contact:Yao Qi, M.D., Chief physician, Master’s supervisor, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China; Chinese PLA General Hospital, Beijing 100853, China -
About author:Zhang Shu-dong, Studying for master’s degree, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China -
Supported by:the Beijing Municipal Science & Technology Commission, No. Z151100003915094
CLC Number:
Cite this article
Zhang Shu-dong1, Zhu Meng-hai1, Li Shi-fei1, Yao Qi1, 2. Sclerostin: a new hope for the treatment of osteoporosis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(36): 5847-5854.
share this article
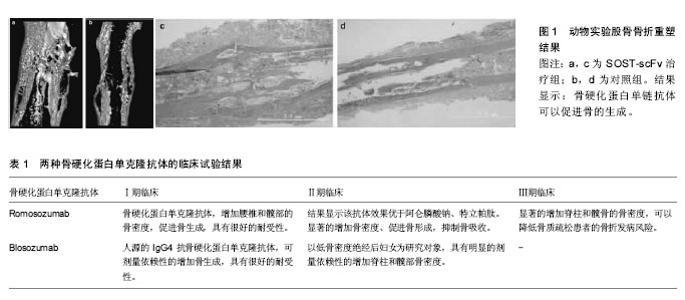
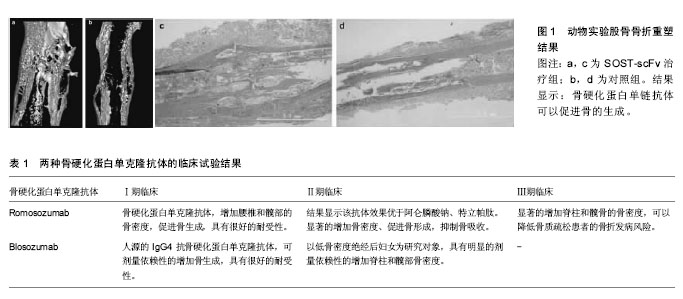
2.1 骨硬化蛋白的来源 骨硬化蛋白是在研究Van Buchem病和Sclerosteosis时发现,由213个氨基酸组成,相对分子质量为24 000,含有一个由23个氨基酸残基组成的分泌信号序列[18-19]。Van Buchem病和Sclerosteosis均是罕见的常染色体隐形遗传病,遗传连锁研究发现,两病的基因均位于染色体17q12-q21[20-21]。 Van Buchem病由Van等在1955年首次描述,最为突出的临床表现是下颌骨增大,颅骨厚度增加。1968年Fosmoe等[22]首次用Van Buchem的名字命名,并沿用至今。Sclerosteosis表现为以骨骼过度生长为特征的硬化性骨发育不良。Balemans等[18]应用定位克隆技术,确定SOST基因是Sclerosteosis患者的突变基因,因其来源于Sclerosteosis而被命名为SOST基因,其编码的蛋白质被称为骨硬化蛋白[22],SOST基因已有3个无义突变、2个剪接点突变、1个错义突变被发现[23]。 Balemans等[24]研究发现Van Buchem病不是SOST基因突变引起,而是因SOST基因下游35 kb区一段 52 kb的片段缺失所致,缺失的片段中隐藏着一个增强子[25]。Sclerosteosis的SOST基因突变和Van Buchem病下游基因片段缺失,导致SOST基因的表达产物骨硬化蛋白缺失[23],而骨硬化蛋白抑制成骨细胞的骨生成,从基因水平解释了两病骨骼过度生长的原因[25]。 2.2 骨硬化蛋白参与骨代谢调节的机制 骨硬化蛋白在骨细胞和成骨细胞中高表达,表达后转运到骨表面发挥功能,强烈的抑制成骨细胞活动的晚期指标—骨矿化结节的生成,只有在高浓度时能轻微的抑制成骨细胞分化的早期指标—ALP(碱性磷酸酶)的活动[23、26],骨硬化蛋白在破骨细胞中不表达,但是能以RANKL依赖的方式刺激破骨细胞分化,间接发挥骨吸收作用[17、25]。骨硬化蛋白通过抑制成骨细胞的分化和功能抑制骨生成,其表达缺失和下调会促进骨的生成,是骨形成的负调节因子[25-26]。 高骨量病(High Bone Mass Disease)和Sclerosteosis都显示出骨细胞和成骨细胞的骨生成功能增加的表现,前者由LRP5(the low density lipoprotein receptor-related protein 5,低密度脂蛋白受体相关蛋白5)基因突变引起,LRP5编码Wnt信号蛋白的一个共受体,Wnt信号通路在骨密度调节中占据核心地位,接受LRP5/6调节[26]。 Mikhail等[26]总结前人经验发现,SOST突变和LRP5突变均可导致骨生成增加;SOST和WISE(结合在Wnt共受体LRP6上并调节Wnt信号的分泌蛋白)存在着相似性,因此提出假设:SOST结合在LRP5/6上,并且抑制经典Wnt通路。 随后,Mikhail等[26]研究证实SOST是Wnt共受体LRP5/6的拮抗性配体,并且是经典Wnt/β-catenin信号的抑制剂。骨硬化蛋白结合在LRP5/6上,通过Wnt信号通路参与骨的调节,LRP5突变可以破坏LRP5和骨硬化蛋白的结合,降低骨硬化蛋白对Wnt信号的抑制作用[23、27]。 Li等[28]研究表明骨硬化蛋白与LRP5上的YWTD-EGF重复区结合,骨硬化蛋白在体外发挥作用时LRP6诱发的Wnt/β-catenin信号通路亦起到重要作用[29]。在体外,骨硬化蛋白通过LRP5起作用,而在体内,该作用机制的证据一直不足[26、28]。 2015年,Yorgan等[30]通过转基因技术使得骨硬化蛋白超表达,首次证明了骨硬化蛋白在体内通过与LRP5结合抑制骨生成。参与骨重塑调节的信号通路有很多,在这些通路中,LRP5/6调节的Wnt信号通路处于核心位置[27]。 生理状态下,Wnt分子结合卷曲蛋白受体(the Frizzled receptor)和LRP5/6共受体,抑制GSK-3β(糖原合成酶激酶-3β),减少β-catenin的磷酸化,导致β-catenin在细胞内累积并转移到细胞核,β-catenin通过T细胞因子和淋巴增强因子激活靶基因的转录,刺激成骨细胞分化,促进骨生成,当Wnt信号缺乏时,β-catenin磷酸化后被泛素识别而泛素化,最终使得β-catenin在蛋白酶体降解,信号传递终止,骨硬化蛋白直接结合在LRP5/6上抑制Wnt通路,抑制成骨细胞的骨生成作 用[17、31]。成骨细胞和破骨细胞在多种因素的调节下,共同维持骨吸收和骨重塑的动态平衡[32],骨硬化蛋白为靶向干预Wnt信号通路治疗骨质疏松提供了新的研究方向。 2.3 骨硬化蛋白在骨质疏松治疗中的应用 2.3.1 骨硬化蛋白单克隆抗体 ⑴骨硬化蛋白单克隆抗体的前临床实验阶段:骨硬化蛋白单克隆抗体的前临床研究开展很多,Li等[33]用去卵巢大鼠建立绝经后骨质疏松模型,建模成功后,给予皮下注射骨硬化蛋白单克隆抗体治疗5周,结果显示,大鼠在骨小梁、骨皮质、骨膜等部位表现出明显的骨生成增加,相比于未去卵巢组,去卵巢组大鼠的骨量、骨强度增加更明显。 Ominsky等[34]第1次将骨硬化蛋白单克隆抗体用于灵长类动物,结果显示猕猴皮下注射骨硬化蛋白单克隆抗体2个月后,在骨小梁和骨皮质产生了显著的合成代谢反应,并且血清中骨合成的标志物迅速的上升、随后下降到基线水平,同血清骨硬化蛋白抗体水平的升降一致。 Virk等[35]将骨硬化蛋白抗体系统化的运用于6 mm标准股骨骨折的大鼠修复模型中,结果显示骨硬化蛋白抗体在大鼠骨折模型中促进骨折愈合,发挥了促合成代谢的作用。大量的研究表明,骨硬化蛋白单克隆抗体应用于动物实验有很好的效果,未见明显不良反应,支持临床试验的开展。 ⑵骨硬化蛋白单克隆抗体的临床试验阶段:骨硬化蛋白单克隆抗体的前临床研究阶段未观测到不良反应,并且能很好促进骨生成,增加骨量、骨密度,抑制骨吸收,可以作为一个可能的治疗骨质疏松的手段应用于临床研究[36]。 为了研究骨硬化蛋白单克隆抗体应用于人体的可能性,并评估该抗体的安全性、可耐受性、药代动力学、药效动力学等指标,Padhi等[36]第1次将AMG785(人源化的骨硬化蛋白单克隆抗体)应用于临床研究。AMG785的临床Ⅰ期试验设计服从随机双盲、安慰剂对照原则,共有72名健康的男性和绝经后女性参与,AMG785和安慰剂(3∶1)皮下(0.1,0.3,1.0,3.0,5.0,10.0mg/kg)或静脉(1.0,5.0 mg/kg)给药。试验中无死亡和治疗终止的事件发生,出现1例非特异性肝炎,已治愈,注射部位反应的发生率高于对照组,与对照组相比,AMG785显著增加腰椎和髋部的骨密度,促进骨生成,抑制骨吸收,有很好的耐受性[36]。数据支持骨硬化蛋白单克隆抗体作为可能的增加骨生成的治疗措施进行下一步临床研究。 Romosozumab (AMG785,人源的骨硬化蛋白单克隆抗体)的临床Ⅱ期试验中,采用多途径、国际性、随机、安慰剂对照原则,设置8个研究组,在419位低骨量的绝经后女性中,分别进行间隔为1个月1次和3个月1次的皮下注射Romosozumap超过12个月。结果显示,不良事件的总发生率在各组之间平衡,相比于其他组,Romosozumap治疗组注射部位反应的发生率增加,治疗组的一小部分药物的安全性不能充分评估[37]。Romosozumab可以快速显著的增加脊柱和髋部的骨密度,促进骨形成,减少骨吸收,效果优于阿仑膦酸钠和特立帕肽对照组,数据支持Romosozumab作为治疗骨质疏松的方法进行第Ⅲ期临床试验[37]。特立帕肽增加骨生成同时增加骨吸收,而Romosozumab增加骨生成的同时抑制骨吸收。Romosozumab和特立帕肽均能增加脊柱和髋骨的骨密度,但Romosozumab效果优于特立帕肽,骨皮质的骨矿化程度亦高于特立帕肽[15],特立帕肽的临床应用有诸多局限,相比之下,Romosozumab的临床应用前景可能会更好[11]。 Romosozumab的Ⅲ期临床试验结果显示,不良反应在试验组和安慰剂组中平衡,注射部位反应温和,在Romosozumab治疗组发生数量较为罕见的下颌骨坏死和不典型股骨骨折、严重的超敏反应,不排除个体差异的作用。在绝经后骨质疏松女性患者中,Romosozumab治疗1年可显著的增加脊柱和髋骨的骨密度,临床骨折的发生风险低于安慰剂组,Romosozumab可以增加骨生成、降低骨吸收[38]。所有的患者在第2年转为地诺单抗治疗,24个月后结果显示,之前接受Romosozumab治疗的组新发椎体骨折的发生率低于安慰剂组。 McColm等[39]将Blosozumab(人源的IgG4抗骨硬化蛋白单克隆抗体)第1次应用于绝经后女性的临床试验中,在Blosozumab的临床Ⅰ期试验中,采用单剂量、多剂量的皮下或静脉给药方式,单剂量和多剂量给药浓度逐渐升至750mg,结果显示,Blosozumab有很好的耐受性,没有安全事件发生,能剂量依赖性的增加骨生成。数据支持Blosozumab作为一种可能的治疗骨质疏松途径进行第Ⅱ期临床试验。 Blosozumab的临床Ⅱ期试验中,120位低骨密度的绝经后妇女加入,皮下注射剂量及间隔为,每4周1次,每次180 mg;每2周1次,每次180 mg;每2周1次,每次270 mg,52周后检测,结果显示,轻微的注射部位反应发生率高于对照组;同对照组相比,治疗组能明显的剂量依赖性的增加脊柱和髋部骨密度[40]。Blosozumab治疗终止1年后对参与试验的女性进行检测,结果显示,结束Blosozuamb的治疗会导致Blosozumab治疗时提升的骨密度下降,但仍高于治疗前的基线水平,骨生成和骨吸收的标志物浓度变化较小[41]。 "
| [1] Lim HS, Kim SK, Lee HH, et al. Comparison in Adherence to Osteoporosis Guidelines according to Bone Health Status in Korean Adult.J Bone Metab.2016;23(3):143-148.[2] Lin X, Xiong D, Peng YQ, et al. Epidemiology and management of osteoporosis in the People's Republic of China: current perspectives.Clin Interv Aging.2015; 25(10): 1017-1033.[3] Hernlund E, Svedbom A, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporosis. 2013;8(1-2):136. [4] Baccaro LF, Conde DM, Costapaiva L, et al. The epidemiology and management of postmenopausal osteoporosis: a viewpoint from Brazil. Clin Interv Aging.2015; 10:583-591.[5] Lötters FJ,Jp VDB,De VF,et al.Current and Future Incidence and Costs of Osteoporosis-Related Fractures in The Netherlands: Combining Claims Data with BMD Measurements.Calcif Tissue Int.2016; 98(3):235-243.[6] Takahara K, Kamimura M, Moriya H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women. Bmc Musculoskelet Disord.2016;17(1):1-7.[7] Chen YC, Lin WC.Can anti-osteoporotic therapy reduce adjacent fracture in magnetic resonance imaging-proven acute osteoporotic vertebral fractures?. Bmc Musculoskelet Disord.2016;17(1):1-5.[8] Hadji P,Jacob L,Kostev K.Gender- and age-related treatment compliance in patients with osteoporosis in Germany.Patient prefer adherence.2016; 10.2379-2385.[9] Chen Z,Arendell L,Aickin M,et al.Hip bone density predicts breast cancer risk independently of Gail score : Results From the Women's Health Initiative.Cancer. 2008; 113(5): 907-15.[10] Mcgraw RL, Riggs JE.Osteoporosis, sedentary lifestyle, and increasing hip fractures: Pathogenic relationship or differential survival bias. Calcif Tissue Int.1994; 55(2):87-89.[11] Shah AD, Shoback D, Lewiecki EM. Sclerostin inhibition: a novel therapeutic approach in the treatment of osteoporosis. Int J Womens Health.2015; 7:565-580.[12] Appelman-Dijkstra NM, Papapoulos SE. Sclerostin Inhibition in the Management of Osteoporosis.Calcif Tissue Int.2016; 98(4):370-380.[13] Yao Q, Ni J, Hou Y, et al.Expression of sclerostin scFv and the effect of sclerostin scFv on healing of osteoporotic femur fracture in rats. Cell Biochem Biophys.2014; 69(2):1-7.[14] Yang X, Deng Z, Wen T, et al. Network Meta-Analysis of Pharmacological Agents for Osteoporosis Treatment and Fracture Prevention. Cell Physiol Biochem. 2016;40(3-4): 781-795.[15] Genant HK, Engelke K,Bolognese MA, et al. Effects of Romosozumab Compared with Teriparatide on Bone Density and Mass at the Spine and Hip in Postmenopausal Women with Low Bone Mass.J Bone Miner Res.2017;32(1):181-187.[16] Lindsay R, Krege JH, Marin F, et al. Teriparatide for osteoporosis: importance of the full course. Osteoporosis Int.2016; 27(8):2395-2410.[17] Hay E,Bouaziz W,Funckbrentano T,et al.Sclerostin and Bone Aging: A Mini-Review. Gerontology.2016;62(6):618-623.[18] Balemans W, Ebeling M, Patel N, et al. Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet.2001; 10(5): 537-543.[19] Balemans W,Van Hul W.Human genetics of SOST.J Musculoskeletal Neuronal Interact.2006; 6(6):355-356.[20] Van HW, Balemans W,Van HE, et al.Van Buchem disease (hyperostosis corticalis generalisata) maps to chromosome 17q12-q21.Am J Hum Genet.1998; 62(2):391-399.[21] Balemans W,Ende JV,Paesalves AF,et al.Localization of the gene for sclerosteosis to the van Buchem disease-gene region on chromosome 17q12-q21. Am J Human Genet.1999; 64(6):1661-1669.[22] Brunkow M. Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein.Am J Human Genet.2001; 64(3):577-589.[23] Piters E, Culha C, Moester M, et al. First missense mutation in the SOST gene causing sclerosteosis by loss of sclerostin function. Hum Mutat.2010; 31(7):E1526–E1543.[24] Balemans W,Patel N,Ebeling M,et al.Identification of a 52 kb deletion downstream of the SOST gene in patients with van Buchem disease. J Med Genet.2002; 39(2):91-97.[25] van Bezooijen RL,Roelen BA,Visser A,et al. Sclerostin Is an Osteocyte-expressed Negative Regulator of Bone Formation, But Not a Classical BMP Antagonist. J Exp Med 2004; 199(6): 805-814.[26] Semënov M,Tamai K,He X.SOST is a ligand for LRP5/LRP6 and a Wnt signaling inhibitor.J Biol Chem.2005; 280(29): 26770-26775.[27] Semenov M V, He X. LRP5 mutations linked to high bone mass diseases cause reduced LRP5 binding and inhibition by SOST.J Biol Chem.2006; 281(50):38276-38284.[28] Li X, Zhang Y, Kang H, et al. Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling.J Biol Chem.2005; 280(20):19883-19887.[29] Chang MK, Kramer I,Keller H,et al.Reversing LRP5-dependent osteoporosis and SOST deficiency-induced sclerosing bone disorders by altering WNT signaling activity. J Bone Miner Res.2014; 29(1):29-42.[30] Yorgan TA,Peters S,Jeschke A,et al.The Anti-Osteoanabolic Function of Sclerostin Is Blunted in Mice Carrying a High Bone Mass Mutation of Lrp5. J Bone Miner Res.2015; 30(7): 1175-1183.[31] Wang Y, Li YP, Paulson C,et al.Wnt and the Wnt signaling pathway in bone development and disease. Front Biosci (Landmark Ed). 2014;19:379-407.[32] Rudnicki MA, Williams BO. Wnt signaling in bone and muscle. Bone.2015; 80:60-66.[33] Li X, Ominsky MS, Warmington KS, et al.Sclerostin antibody treatment increases bone formation, bone mass, and bone strength in a rat model of postmenopausal osteoporosis. J Bone Miner Res.2009; 24(4):578-588.[34] Ominsky MS,Vlasseros F,Jolette J,et al.Two doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strength. J Bone Miner Res.2010; 25(5):948-959.[35] Virk MS, Alaee F, Tang H, et al.Systemic Administration of Sclerostin Antibody Enhances Bone Repair in a Critical-Sized Femoral Defect in a Rat Model.J Bone Joint Surg Am.2013; 95(8):694-701.[36] Padhi D, Jang G, Stouch B, et al. Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Miner Res.2011; 26(1):19-26.[37] McClung MR,Grauer A,Boonen S,et al.Romosozumab in Postmenopausal Women with Low Bone Mineral Density.N Enl J Med.2014;370:412-420.[38] Cosman F,Crittenden DB,Adachi JD,et al.Romosozumab Treatment in Postmenopausal Women with Osteoporosis.New Engl J Med.2016; 375(16):1532-1543.[39] Mccolm J,Hu L,Womack T,et al.Single- and multiple-dose randomized studies of blosozumab, a monoclonal antibody against sclerostin, in healthy postmenopausal women. J Bone Miner Res.2014; 29(4):935–943.[40] Recker R,Benson C,Matsumoto T,et al.A randomized, double-blind phase 2 clinical trial of blosozumab, a sclerostin antibody, in postmenopausal women with low bone mineral density.J Bone Miner Res.2015; 30(2):216-224.[41] Recknor CP, Recker RR, Benson CT, et al.The Effect of Discontinuing Treatment With Blosozumab: Follow-up Results of a Phase 2 Randomized Clinical Trial in Postmenopausal Women With Low Bone Mineral Density.J Bone Miner Res. 2015; 30(9):1717-1725.[42] Claire MN, Patton D,Hayes JS.Sclerostin Antibody Therapy for the Treatment of Osteoporosis: Clinical Prospects and Challenges.J Osteoporosis.2016;2016(6217286).[43] Sugiyama T, Torio T, Miyajima T, et al. Romosozumab and Blosozumab: Alternative Drugs of Mechanical Strain-Related Stimulus Toward a Cure for Osteoporosis. Front Endocrinol (Lausanne). 2015; 6:54.[44] Florio M,Gunasekaran K,Stolina M,et al.A bispecific antibody targeting sclerostin and DKK-1 promotes bone mass accrual and fracture repair. Nat Commun. 2016;7:11505.[45] Boschert V, Frisch C, Back JW, et al.The sclerostin- neutralizing antibody AbD09097 recognizes an epitope adjacent to sclerostin's binding site for the Wnt co-receptor LRP6. Open Biol. 2016;6(8). pii: 160120. [46] Basha G, Ordobadi M, Scott W R, et al. Lipid Nanoparticle Delivery of siRNA to Osteocytes Leads to Effective Silencing of SOST and Inhibition of Sclerostin In Vivo. Molecular Therapy- Nucleic Acids.2016; 5(9):e363.[47] Armamento-Villareal R,Sadler C,Napoli N,et al.Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. J Bone Miner Res.2012; 27(5):1215-1221.[48] Gombos GC, Bajsz V, Pék E, et al. Direct effects of physical training on markers of bone metabolism and serum sclerostin concentrations in older adults with low bone mass. Bmc Musculoskelet Disord.2016;17(1):1-8.[49] Ardawi MS, Rouzi AA, Qari MH. Physical Activity in Relation to Serum Sclerostin, Insulin-Like Growth Factor-1, and Bone Turnover Markers in Healthy Premenopausal Women: A Cross-Sectional and a Longitudinal Study.J Clin Endocrinol Metab.2012;97(10):3691-3699.[50] Compton JT, Lee FY. A review of osteocyte function and the emerging importance of sclerostin.J Bone Joint Surg Am.2014; 96(19):1659-1668.[51] Spatz JM, Fields EE, Yu EW, et al.Serum sclerostin increases in healthy adult men during bed rest.J Clin Endocrinol Metabo.2012; 97(9):1736-1740.[52] Zagrodna A,Jó?ków P,M?dra? M,et al.Sclerostin as a novel marker of bone turnover in athletes. Biol Sport.2016; 33(1): 83-87.[53] Christen P, Ito K, Ellouz R, et al. Bone remodelling in humans is load-driven but not lazy. Nat Commun.2014; 5(5): 4855-4855.[54] Galea GL, Lanyon LE, Price JS. Sclerostin's role in bone's adaptive response to mechanical loading.Bone.2017; 96: 38-44.[55] Robling AG, Niziolek PJ, Baldridge LA,et al.Mechanical stimulation of bone in vivo reduces osteocyte expression of Sost/sclerostin.J Biol Chem.2008; 283(9):5866-5875.[56] Silverman SL.Sclerostin. J Osteoporos.2010;2010:941419[57] Gupta A,March L.Treating osteoporosis.Australian Prescriber. 2016;39(2):40-46. [58] Thouverey C,Caverzasio J.Sclerostin inhibits osteoblast differentiation without affecting BMP2/SMAD1/5 or Wnt3a/β-catenin signaling but through activation of platelet-derived growth factor receptor signaling in vitro. Bonekey Rep.2015; 4:757. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhou Qian, Zhang Qiang, Chen Qiu. Human salivary components and osteoporosis/osteopenia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1439-1444. |
| [4] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [5] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [6] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [7] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [8] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [9] | Peng Kun. Improvement of the treatment effect of osteoporotic fractures: research status and strategy analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 980-984. |
| [10] | Shen Song, Xu Bin. Diffuse distribution of bone cement in percutaneous vertebroplasty reduces the incidence of refracture of adjacent vertebral bodies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 499-503. |
| [11] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [12] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [13] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [14] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [15] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||