Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (8): 1215-1220.doi: 10.3969/j.issn.2095-4344.2017.08.012
Previous Articles Next Articles
Fixed bite plate combined with intermaxillary traction screw for free fibula flap repair of mandibular defects
Zhou He-jie, Xu Xiao-mei, Mao Jie, Zhou Yi-fei
- Hospital of Stomatology, Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2017-01-17Online:2017-03-18Published:2017-04-14 -
Contact:Xu Xiao-mei, M.D., Associate professor, Hospital of Stomatology, Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Zhou He-jie, Studying for master’s degree, Attending physician, Hospital of Stomatology, Southwest Medical University, Luzhou 646000, Sichuan Province, China -
Supported by:the Scientific and Technologic Program of Sichuan Province, No. 2015JY0199
CLC Number:
Cite this article
Zhou He-jie, Xu Xiao-mei, Mao Jie, Zhou Yi-fei. Fixed bite plate combined with intermaxillary traction screw for free fibula flap repair of mandibular defects[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(8): 1215-1220.
share this article
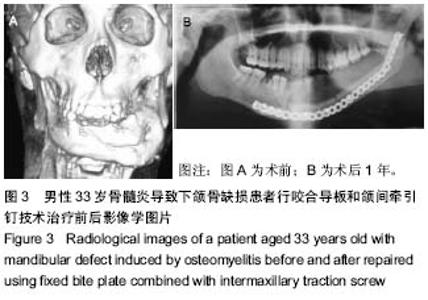
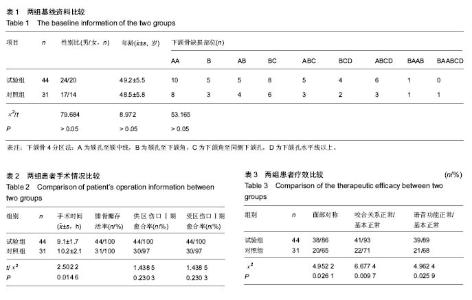
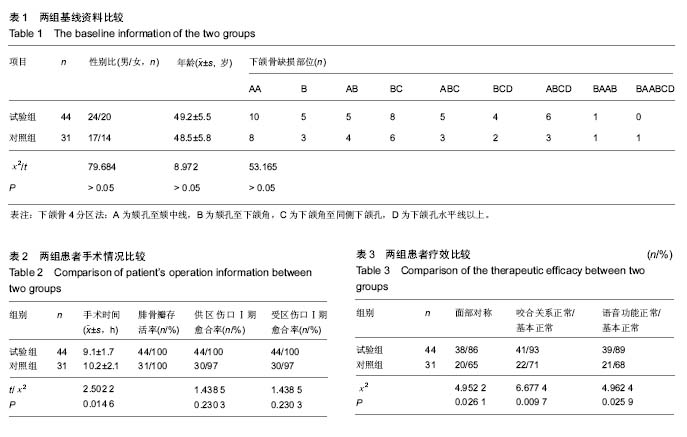
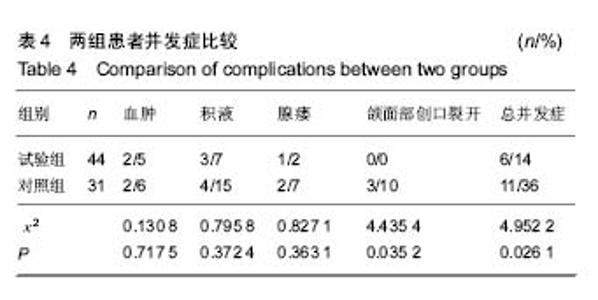
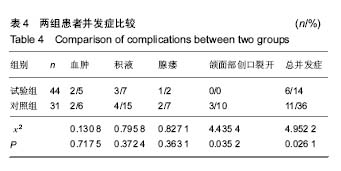
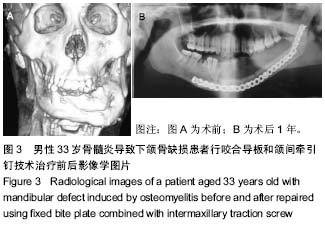
2.3 两组患者手术情况比较 2组患者平均手术时间差异有显著性意义(P < 0.05)。试验组44例患者移植的腓骨瓣均成功,且供区、受区切口均是Ⅰ期愈合;对照组31例患者移植的腓骨瓣均成功,30例患者受区Ⅰ期愈合,30例患者供区伤口Ⅰ期愈合。腓骨瓣移植成功率、受区切口Ⅰ期愈合率以及供区伤口Ⅰ期愈合率两者比较差异无显著性意义(P > 0.05),详见表2。 2.4 两组患者疗效比较 所有患者术后均进行随访,时间为8-24个月。试验组38例患者面部恢复对称,41例患者咬合关系正常/基本正常,39例患者语音功能正常/基本正常;对照组20例患者面部恢复对称,22例患者咬合关系正常/基本正常,21例患者语音功能正常/基本正常,以上差异均有显著性意义(P < 0.05),详见表3。 2.5 两组患者并发症比较 所有患者供区无明显运动及感觉障碍,术后均可以正常行走。受区试验组总并发症发生率为14%,其中血肿2例,积液3例,腺瘘1例,颌面部创口裂开0例;对照组总并发症发生率为36%,其中血肿2例,积液4例,腺瘘2例,颌面部创口裂开3例。2组患者在总并发症发生率及颌面部创口裂开率上差异有显著性意义(P < 0.05),其余差异无显著性意义,详见表4。 2.6 典型病例 男性,33岁,诊断为骨髓炎导致下颌骨缺损,行咬合导板和颌间牵引钉技术治疗,随访12个月,无不良事件发生,见图3。"
| [1] 曲行舟,王明一,马继壮,等. 上颌翼状导板在上下颌骨联合缺损早期赝复治疗中的应用[J]. 上海口腔医学,2010,19(2):133-135.[2] Karagoz H,Eren F,Sever C,et al. Mandibular reconstruction after hemimandibulectomy. J Craniofac Surg. 2012;23(5): 1373-1374. [3] Hayden RE,Mullin DP,Patel AK. Reconstruction of the segmental mandibular defect: current state of the art. Curr Opin Otolaryngol Head Neck Surg. 2012;20(4): 231-236. [4] Politi M,Toro C. Iliac flap versus fibula flap in mandibular reconstruction. J Craniofac Surg. 2012;23(3): 774-779. [5] 贾暮云,蒋济金,初晓艺,等. 下颌骨缺损重建板修复术后十年回顾性分析[J]. 中华口腔医学杂志,2016,51(7):43-45.[6] 王玉龙,韩龙,毛驰. 下颌骨缺损的修复重建[J]. 口腔颌面修复学杂志,2011,12(2):126-128.[7] Hidalgo DA. Fibula free ap: a new method of mandible reconstruction. Plast Reeonstr Surg. 1989;84(1): 71-79. [8] 汤晶,葛自力,祝华珺,等. 牵引钉植入与牙弓夹板行颌间牵引固定治疗单纯髁状突骨折的疗效比较[J]. 口腔医学, 2015,35(6): 468-472.[9] 谭繁胜,赵建红,谭海波,等.颌间牵引钉联合微型钛板内固定在颌骨骨折治疗中的应用[J].现代口腔医学杂志,2012,26(6):366-369.[10] 杨福彪,常克武,徐德衡. 浅谈腓骨瓣修复下颌骨缺损[J]. 中外健康文摘,2011,8(18):159-160.[11] 张熙恩,李自力,陈波. 双颌板技术在正颌外科中的应用. 中华口腔医学杂志,2001,36(1): 73-75. [12] 段银钟,孙应明,顾晓明,等. 各种咬合导板在正畸正颌中的应用[J]. 口腔颌面外科杂志,2001,11(s1):24-25.[13] 常永春, 郭杰. 深覆患者弹性颌平面导板矫治后下前牙牙根吸收情况观察[J]. 山东医药,2015,55(27):66-67.[14] 胡超, 王建华, 张纲,等. 颌间牵引钉联合微型钛板内固定在颌骨骨折治疗中的应用[J]. 中国医药导刊,2014,(3):393-394.[15] 王秦宁,宋治锋. 颌间牵引钉与微型钛板在颌骨骨折中的临床应用[J]. 创伤外科杂志,2010,12(5):455-455.[16] Lundgren TK,Pignatti M,Halle M,et al. Composite orbital reconstruction using the vascularized segmentalized osteo-fascio-cutaneous fibula flap. J Plastic Reconstructive Aesthetic Surg. 2015;69(2):255-261.[17] 冯琴,吴贤慧,秦丽英. 前臂皮瓣复合腓骨瓣修复下颌骨缺损术的围手术期护理[J]. 现代临床护理,2014,(1):49-52.[18] Halim AS,Chai SC,Wan IW,et al. Long-term outcome of free fibula osteocutaneous flap and massive allograft in the reconstruction of long bone defect. J Plastic Reconstructive Aesthetic Surg. 2015;68(12):1755-1762.[19] 范亚伟,齐鸿亮,范慧芳,等.计算机导航技术在下颌骨缺损种植修复重建的临床研究[J]. 中国药物与临床,2015,15(7):909-911.[20] Kim JW, Hwang JH, Ahn KM. Fibular flap for mandible reconstruction in osteoradionecrosis of the jaw: selection criteria of fibula flap. Maxillofac Plast Reconstr Surg. 2016; 38(1):46.[21] Shroff SS,Nair SC,Shah A,et al. Versatility of Fibula Free Flap in Reconstruction of Facial Defects: A Center Study. J Maxillofac Oral Surg. 2016:1-7.[22] 张朕坡. 组织工程骨修复下颌骨缺损研究进展[J]. 中华实用诊断与治疗杂志,2015,29(10):949-951.[23] Bouyer M,Corcella D,Forli A,et al. Lower limb salvage with a free fillet fibula flap harvested from the contralateral amputated leg. Ann Chir Plast Esthet. 2015;60(3):247-251.[24] 陆建荣,班华杰,王代友,等. 血管化游离腓骨肌皮瓣修复下颌骨缺损的临床观察[J]. 中华临床医师杂志:电子版,2014,8(19): 3578-3581.[25] Sinno S,Rodriguez ED. Nuances and Pearls of the Free Fibula Osteoseptocutaneous Flap for Reconstruction of a High-Energy Ballistic Injury Mandible Defect. Plast Reconstr Surg. 2016;137(1):280.[26] 章臻,潘巨利,黄欣,等. 下颌骨缺损的个体化修复重建[J]. 口腔颌面外科杂志,2014,24(4):293-296.[27] Basat SO,Örero?lu AR,Orman C,et al. Recurrent Ameloblastoma in the Free Fibula Flap: Review of Literature and an Unusual Case Report. J Maxillofac Oral Surg. 2015; 14(3):821-825. [28] 钟建鑫,节云峰,罗金英,等. 多孔钽颗粒在下颌骨缺损修复中的作用[J]. 第三军医大学学报,2015,37(12):1277-1280.[29] 赵虹,连白玲,杨金玉. 血管化腓骨肌皮瓣重建下颌骨缺损的护理[J]. 现代医药卫生,2014,30(1):98-99.[30] 颜光启,王雪,谭学新,等. 应用SurgiCase软件指导游离腓骨皮瓣修复下颌骨缺损的研究[J]. 中国修复重建外科杂志,2013, 27(8):1006-1009.[31] 陈旭兵,柳兆刚,袁建兵,等. 三维模拟技术在游离腓骨瓣移植重建下颌骨缺损中的应用[J]. 上海口腔医学,2015,24(4):460-464.[32] 陈勇,杨旭东,李威,等. 计算机辅助三维可视化技术在腓骨瓣修复下颌骨缺损中的应用[J]. 中华显微外科杂志, 2013,36(1): 19-23.[33] 邓娜,何巍,付坤,等. 数字化外科在游离腓骨瓣修复下颌骨缺损中的应用[J]. 河南外科学杂志,2015,(3):12-15.[34] 杨志诚,向旭,严颖彬,等. 咬合导板及颌间牵引钉技术在游离腓骨瓣修复下颌骨缺损中的应用[J]. 中国修复重建外科杂志, 2013,27(3):292-294.[35] 佟猛,李龙江,温玉明,等. 带血管蒂腓骨组织瓣游离移植修复下颌骨缺损的临床研究[J]. 华西口腔医学杂志,2002,20(5): 340-342.[36] 栾修文,艾伟健,刘曙光,等. 游离腓骨肌(皮)瓣在下颌骨缺损修复重建中的应用[J]. 广东牙病防治,2008,16(4):180-182.[37] 邓永强,郑苍尚,朱耀旻,等. 腓骨及髂骨组织瓣在修复下颌骨缺损的应用比较研究[J]. 口腔医学研究,2013,29(6): 569-571.[38] 马征,舒伟,李彪,等. 血管化腓骨复合组织瓣在下颌骨缺损修复重建中的初步应用[J]. 药物与人,2014,35(5):22-22.[39] 孙宾,于子莹,邵海峰,等. 游离腓骨肌皮瓣修复下颌骨缺损的临床应用及其治疗效果评价[J]. 吉林大学学报(医学版),2014, 40(6): 1285-1288.[40] 白振西,高志彪,肖霞,等. 颌间牵引钉在颌骨骨折内固定手术治疗中的临床应用研究[J]. 实用口腔医学杂志,2015,(2):219-224.[41] Eser C,Gencel E,Kesikta? E,et al. Outcomes of Anatomic Reconstruction of Gunshot-Inflicted Lower Face Defects by Free Osteoseptocutaneous Fibula Flap and Expanded or Nonexpanded Temporal Scalp Flap Combination in Males. J Craniofac Surg. 2016;27(5):1139-1142. [42] Man QW,Jia J,Liu K,et al.Secondary reconstruction for mandibular osteoradionecrosis defect with fibula osteomyocutaneous flap flowthrough from radial forearm flap using stereolithographic 3-dimensional printing modeling technology. J Craniofac Surg. 2015;26(2):e190-193. [43] Diaz-Carandell A,Agut-Busquet E,Molina-Montes J,et al. Intraoral Approach and Stereolithographic-guided Large Mandibular Reconstruction with Fibula Free Flap. Plast Reconstr Surg Glob Open. 2014;2(8):e199. [44] Dorafshar AH,Mundinger GS,Mohan R,et al. Comparison of free fibular flaps with reamer-irrigator-aspirator bone grafts for the reconstruction of critical-sized mandibular defects. J Craniofac Surg. 2014;25(6):1953-1958. [45] Hillerup S,Elberg JJ,Thorn JJ,et al. Reconstruction of irradiated mandible after segmental resection of osteoradionecrosis-a technique employing a microvascular latissimus dorsi flap and subsequent particulate iliac bone grafting. Craniomaxillofac Trauma Reconstr. 2014 S;7(3): 190-196. [46] Yang Z,Xiang X,Yan Y,et al. [Application of occlusal guide plate combined with intermaxillary fixation screw in mandibular defect repair with free fibular flap]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27(3):292-294. [47] Bartaire E,Mouawad F,Mallet Y,et al. Morphologic assessment of mandibular reconstruction by free fibula flap and donor-site functional impairment in a series of 23 patients. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129(5):230-237. [48] Dean NR,Wax MK,Virgin FW,et al. Free flap reconstruction of lateral mandibular defects: indications and outcomes. Otolaryngol Head Neck Surg. 2012;146(4):547-552. [49] Poglio G,Grivetto F,Nicolotti M,et al. Management of an exposed mandibular plate after fibula free flap with vacuum-assisted closure system. J Craniofac Surg. 2011; 22(3):905908.[50] Kuo YR,Shih HS,Chen CC,et al. Free fibula osteocutaneous flap with soleus muscle as a chimeric flap for reconstructing mandibular segmental defect after oral cancer ablation. Ann Plast Surg. 2010;64(6):738-742 |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [3] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [4] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [5] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [6] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [7] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [8] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [9] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [10] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [11] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [12] | Chen Jinmin, Chen Suisheng, Ding Jing, Xia Baoquan, Luo Xiaojia, Lu Chenghai. Stability of balloon dilation with injectable calcium sulfate cement for tibial plateau fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 414-418. |
| [13] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [14] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||