Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (30): 5518-5524.doi: 10.3969/j.issn.2095-4344.2013.30.016
Previous Articles Next Articles
Bernese periacetabular osteotomy for the treatment of acetabular dysplasia
Song Li-ming
- Department of Joint Surgery, Tianjin Hospital, Tianjin 300211, China
-
Received:2013-04-09Revised:2013-05-07Online:2013-07-23Published:2013-07-23 -
About author:Song Li-ming★, Master, Attending physician, Department of Joint Surgery, Tianjin Hospital, Tianjin 300211, China sososlm@126.com
CLC Number:
Cite this article
Song Li-ming. Bernese periacetabular osteotomy for the treatment of acetabular dysplasia[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(30): 5518-5524.
share this article

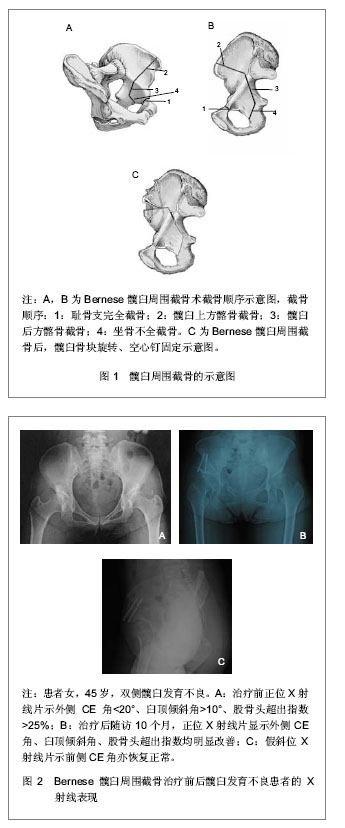
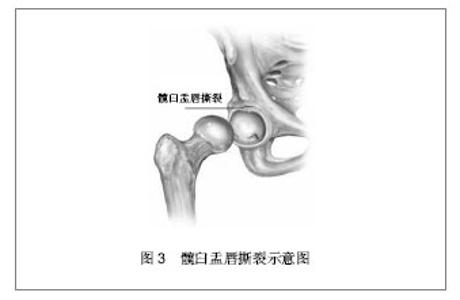
2.1 纳入文献基本情况 共纳入43篇文献,均涉及Bernese髋臼周围截骨的手术适应证及技术和影响疗效的因素。 2.2 Bernese髋臼周围截骨的指征 Bernese髋臼周围截骨最适合于青少年和青年髋臼发育不良患者。如果近期MRI显示有轻度软骨损伤、患者强烈要求保留关节,并且术者非常熟悉髋臼周围截骨手术,则可以将手术患者年龄放宽至50岁[2]。当然,决定年龄上限时也要将截骨手术效果与人工关节置换效果进行比较。 Bernese髋臼周围截骨的手术指征包括:①患者行走及劳累时有髋关节疼痛或疲劳症状。②髋关节骨关节炎Tönnis 0期、Ⅰ期患者,或有较轻症状的Tönnis Ⅱ期患者。③髋臼和股骨头形状有足够的吻合度。④有髋臼外侧CE角小于20°、髋臼顶倾斜角小于10°、前方CE角小于20°、股骨头超出指数大于25%其中至少一项。⑤髋关节能充分屈曲(≥100°)、外展(≥30°),不需行股骨近端成形术。当然,对于年轻患者,手术指征可以适当放宽,以免软骨进一步损伤而影响预后。 Bernese髋臼周围截骨术的禁忌证包括:①严重的关节退变性疾病。②年龄超过65岁。③患髋活动度明显受限的患者。④髋臼和股骨头形状差异较大。⑤肥胖患者。⑥伴有严重的内科合并症。⑦患者不配合。 2.3 Bernese髋臼周围截骨治疗的技术方法 在Bernese截骨术临床应用的最初几年中,需要将外展肌群从髂骨翼上剥离,以便于髂骨的V形截骨,不过现在所有截骨都是在骨盆内侧进行的,从而不需要再剥离外展肌群[2,7-9]。 2.3.1 手术入路 通常采用改良Smith-Peterson入路[2],将髂前上棘及缝匠肌止点自髂骨上凿断并向内侧翻转。分离髋关节前内关节囊和腰大肌之间的间隙,显露坐骨,直至闭孔外肌近侧。此时应非常小心,因为旋股内侧动脉就位于闭孔外肌远侧,应避免损伤。 也有人采用髂腹股沟入路[1]。切口从髂嵴前1/3至耻骨联合上方2 cm处,游离并保护股外侧皮神经。切开髂嵴骨膜,骨膜下剥离髂骨内板至坐骨大切迹,纱布填塞止血。继续骨膜下剥离至四边体、坐骨棘、闭孔内下缘。切开腹股沟管,保护子宫圆韧带或精索,切断腹股沟韧带,分离股神经与股血管鞘间隙。在腹直肌止点上1 cm处横断腹直肌前、后鞘,显露并切开耻骨支骨膜,分离耻骨支与膀胱前间隙,触及闭孔内、下缘。 改良Smith-Peterson切口的优点是操作时间短,便于旋转髋臼骨块,而且能够显露前关节囊,便于处理关节内病变。缺点是容易造成股外侧皮神经麻痹[10],容易引起异位骨化,切口瘢痕不美观,而且坐骨截骨无法直视下完成,只能借助X射线透视。 而髂腹股沟入路是显露骨盆内壁最直接的入路,能够直视下行坐骨截骨[11],截骨部位准确、安全、彻底,而且容易控制截骨线、截骨量和髋臼骨块旋转角度,对于骨盆发育明显畸形的患者尤其适合。髋臼上部骨组织的血运主要来自髂骨外板臀上动脉的分支髋臼上动脉和髋臼动脉。因此采用髂腹股沟入路对髋臼的血运破坏小,髋臼骨块坏死率低。除此之外,此入路引起股外侧皮神经麻痹的概率低,而且髂骨外板肌肉剥离少,异位骨化发生率低。缺点是:此入路无法进入关节腔,无法处理关节内问题;容易引起血管并发症,包括淋巴管断裂、继发血肿、淋巴水肿、股动脉或髂动脉栓塞等[2]。 2.3.2 髋臼周围截骨步骤 髋臼周围截骨共分4步:第1步是坐骨的不全截骨,起自髋臼下沟(髋臼的后下缘),使用特殊骨刀截骨,通常深度为2.0-2.5 cm。建议截骨时用手触摸骨性标志,当然也有许多术者采用X射线透视监控截骨方向。第2步是髂耻隆起内侧的耻骨完全分离截骨。注意必须用钝头拉钩保护闭孔神经和血管。第3步截骨又分为两部分,即用摆锯行髋臼上方截骨和用骨刀行髋臼后方截骨。第4步截骨是从骨盆内侧用特殊骨刀连接第1步坐骨不全截骨线和第3步髋臼后方截骨线[9,12-13]。 截骨后,自髂前下棘处旋入一枚斯氏针作为把持器,并使用扩张器控制髋臼骨块,以改变髋臼朝向。矫正髋臼骨块位置时,最好先向前旋转骨块,这样通常还能够同时增加外侧覆盖率,如尚需进一步增加外侧覆盖率,还可以再旋入1枚斯氏针作为保持器。但是如果先向外旋转骨块增加外侧覆盖率,则会造成骨块和骨床之间早期就出现很高的摩擦力,从而使其他操作较为费力。髋臼骨块旋转后,拍摄X射线平片以更好的控制髋臼的空间矫正程度,最后用3枚3.5 mm螺钉固定骨块,见图1,2。"
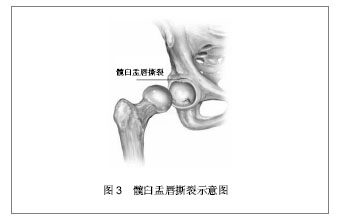
另外,特别应注意一些患者治疗前就存在髋臼后倾[14]。髋臼后倾除了见于髋臼发育不良,更常见于无发育不良的髋关节,患者治疗前可能就存在有髋臼撞击症的表现。对于伴有髋臼后倾的髋关节发育不良就不单纯是髋臼的问题,而是一种半骨盆的扭转问题[15-16]。髋臼后倾引起的单纯撞击是髋臼前侧过度覆盖区域与股骨头颈交界处之间的线性接触。不过,许多额状面覆盖正常但有髋臼后倾的髋关节同时存在股骨近端畸形,主要是股骨头非球形的突起[17]。对于髋臼后倾的年轻患者,如果软骨缘无严重损伤并且髋臼后缘位于旋转中心内侧,则应当行反向髋臼周围截骨治疗[18],这样通过内旋髋臼骨块重建髋臼前倾[19],以避免髋臼前侧撞击。不过随着髋臼前倾矫正角度的增加,髋臼后侧撞击的风险也会增加,而且单纯前关节囊切开也难以纠正股骨近端的严重畸形。对于这种病例,治疗者可以考虑先经外侧入路行股骨近端成形术。然后根据局部情况,通过此入路进一步进行髋臼缘修整或髋臼周围截骨[20]。需要注意的是,如果经外侧入路行髋臼周围截骨并且广泛切开了关节囊,那么一定要保护髋臼骨块的血供[21]。 对于髋关节发育不良患者进行髋臼周围截骨治疗时,除了可以采用常规单一手术切口外,还有另外一种可行的办法,也就是先通过外侧入路仅进行髋臼周围截骨术的第一步,也是最难的坐骨截骨,然后将患者放平至仰卧位,再通过Smith-Peterson入路进行其他的髋臼周围截骨。这样手术比较安全,而且手术时间也较短。采用这种方法,如果手术中将Smith-Peterson入路向腹股沟延伸,则可用以处理复杂凸起性髋关节或年轻患者的创伤后髋臼骨盆内脱位[22]。 2.4 Bernese髋臼周围截骨后的处理 Bernese髋臼周围截骨术后,根据截骨的矫正程度和患者的恢复情况,通常需卧床休息6-8周,复查X射线片,然后可以逐渐增加髋关节下地负重和肌肉力量,开始活动度锻炼。再经过三四周部分负重练习后就可以正常使用患髋了。 2.5 Bernese髋臼周围截骨的预后及影响因素 2.5.1 髋关节退变和髋关节发育不良的严重程度 影响Bernese髋臼周围截骨术后效果的直接因素是术前影像学上髋关节退变和发育不良的严重程度。Siebenrock等[3]在对75例患者随访10年后发现,如果仅评估不存在骨性关节炎的病例,则术后结果良好的病例占88%,如果所有病例都包括在内,则结果良好的病例降至73%。随访20年后,此两组患者的成功率分别为75%和60%,这同时也表明髋臼周围截骨是一种成功的治疗髋关节发育不良的方法,而且其远期结果优于股骨截骨矫形治疗。 与股骨截骨矫形类似,对于髋关节骨性关节炎达到Tönnis Ⅲ期的患者,髋臼周围截骨术的失败率很高。因此,这类病例不是髋臼周围截骨术的适应证。不过,患者术前的前后位X射线片有时可能会误导术者,因为股骨头向前外侧半脱位在X射线片上可以造成髋关节间隙变窄的假象。这时应当外展并轻度屈髋,如果髋关节关节间隙明显增宽,则此髋仍可以行髋臼周围截骨术,并且几年内预后都会很好。 2.5.2 年龄 对于年龄是否影响术后效果仍存在争议。有些研究显示患者年龄超过40岁,手术预后不良[23-25]。但是另外的研究发现患者年龄超过55岁同样可以取得良好效果[26],不过需要注意的是此高龄组患者关节面吻合度必须良好,并且没有或仅有轻度退变。Leunig等[2]认为如果近期MRI显示髋关节仅有轻度软骨损伤、患者要求保守治疗并且术者髋臼周围截骨经验非常丰富,那么患者年龄可以放宽到50岁,其结果同样满意。Millis等[27]也认为对于40岁以上且仅有轻度或没有关节炎表现的髋臼发育不良患者,髋臼周围截骨术可以获得满意的功能及疼痛评分,而且他们也发现术前关节炎严重程度似乎比年龄对术后疗效的影响更大。 2.5.3 髋臼后倾 随着认识的深入,发现髋臼发育不良患者不完全都是股骨头前外侧覆盖不足,而是单一或联合的前侧、外侧及后侧覆盖问题,特别是1/6的病例可能表现为髋臼后倾[28]。显著的髋臼后倾主要是见于纠正髋臼朝向的手术后,例如儿童期的Salter截骨后[29],也可见于伴有股骨近端局灶性缺损的髋关节发育不良[30]、创伤后发育不良[31]。对于后倾型髋关节发育不良髋臼,如果采用与前-外侧发育不良髋臼相同的矫正方法,则会加重髋关节病变,将来难免需要行非常复杂的翻修手术。这时就需要行反向髋臼周围截骨术,并且需注意避免矫枉过正。 2.5.4 截骨后的髋臼撞击症 Siebenrock等[3]在随访10年后发现了一种未曾预料到的结果:有近30%患者出现了撞击症状,即使是髋臼周围截骨术后髋臼朝向已非常好的患者。进一步的研究显示在所有髋臼发育不良病例中,多数患者前侧股骨头-颈交界处经常没有腰形曲度,所以在髋臼矫正后,会最终导致髋臼前缘与股骨头-颈交界处撞击[32]。因此,需要常规行髋关节囊切开术以检查髋关节活动度,特别是内旋时髋臼前缘有无撞击,必要时还要行股骨头颈处骨-软骨成形术以恢复前-外侧头颈曲度。当然对于发育不良的髋关节,行髋臼和股骨的联合矫形术应该会取得更好的结果,但是目前这种联合手术的例数还比较少[33-34],经验还不足。 Ziebarth等[35]在对一组38例(46髋)行髋臼周围截骨患者平均随访12个月后也发现,尽管所有患者截骨后股骨头覆盖良好,但是其中19例患者出现了明显的髋臼撞击的表现。他们认为髋臼周围截骨后髋臼撞击症的发生率很高,而且男性患者的发生率更高一些。而如何降低撞击症的发生率还有待进一步研究。 2.5.5 髋臼盂唇病变情况 Leunig等[2]在早期研究中就发现髋臼缘存在着各种不同的病变情况。众所周知,髋关节发育不良可以伴有盂唇撕裂[36],见图3。常规MRI更容易发现这一病变[37],而且同时还常伴有其他臼缘病变,例如关节囊内、外的囊肿形成。也有学者将发育不良髋关节出现的臼缘骨折定义为一种特殊类型的臼缘撕裂[38]。通过MRI,有时会发现盂唇撕裂深入到髋臼软骨内,造成软骨不连续。有学者认为,相对于盂唇自软骨边缘撕裂的情况,这种情况的预后更加不好。Siebenrock等[3]通过10年随访也发现,手术时盂唇完整的髋关节比盂唇撕裂的临床效果好。髋臼发育不良的另外一种臼缘病变是盂唇肥厚,这时髋关节的症状可能主要是撞击引起的,而不是髋关节发育不良引起的[39]。"
| [1] Okano K, Enomoto H, Osaki M, et al. Outcome of rotational acetabular osteotomy for early hip osteoarthritis secondary to dysplasia related to femoral head shape: 49 hips followed for 10-17 years. Acta Orthop. 2008;79(1):12-17.[2] Leunig M, Ganz R. Mini-symposium: children-osteotomies around the hip:(iii)Bernese periacetabular osteotomy. Current Orthopaedics. 2007;21(2):100-108.[3] Siebenrock KA, Schöll E, Lottenbach M, et al. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999; (363): 9-20.[4] Kralj M, Mavcic B, Antolic V, et al. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7-15-year follow-up of 26 hips. Acta Orthop. 2005;76(6):833-840.[5] Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop. 2005;76(1): 67-74.[6] Clohisy JC, Barrett SE, Gordon JE, et al. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87(2):254-259.[7] Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88(9): 1920-1926.[8] Steppacher SD, Tannast M, Ganz R, et al. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466(7):1633-1644.[9] Hussell JG, Mast JW, Mayo KA, et al. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999;(363):64-72.[10] Kiyama T, Naito M, Shiramizu K, et al. Ischemia of the lateral femoral cutaneous nerve during periacetabular osteotomy using Smith-Petersen approach. J Orthop Traumatol. 2009; 10(3):123-126.[11] Pogliacomi F, Stark A, Vaienti E, et al. Periacetabular osteotomy of the hip: the ilioinguinal approach. Acta Biomed. 2003;74(1):38-46.[12] Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;(363):21-32.[13] Ganz R, Leunig M. Twenty years of experience with the Bernese periacetabular osteotomy for residual acetabular dysplasia. Treatment of osteoarthritic change in the hip. 2007: 147-161. [14] Lequesne M, Bellaïche L. Anterior femoroacetabular impingement: an update. Joint Bone Spine. 2012;79(3): 249-255.[15] Jamali AA, Mladenov K, Meyer DC, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the "cross-over-sign". J Orthop Res. 2007;25(6): 758-765.[16] Kalberer F, Sierra RJ, Madan SS, et al. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677-683.[17] Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7): 1012-1018.[18] Philippon MJ, Wolff AB, Briggs KK, et al. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26(6):757-761.[19] Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278-286.[20] Leunig M, Rothenfuh D, Beck M, et al. Surgical dislocation and periacetabular osteotomy through a posterolateral approach: a cadaveric feasibility study and initial clinical experience. Oper Tech Orthop. 2004;14(2):49-57.[21] Beck M, Leunig M, Ellis T, et al. The acetabular blood supply: implications for periacetabular osteotomies. Surg Radiol Anat. 2003;25(5-6):361-367.[22] Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res. 2010;468(12):3168-3180.[23] De La Rocha A, Sucato DJ, Tulchin K, et al. Treatment of adolescents with a periacetabular osteotomy after previous pelvic surgery. Clin Orthop Relat Res. 2012;470(9): 2583-2590.[24] Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty. 2008;23(7):960-963.[25] Teratani T, Naito M, Kiyama T, et al. Periacetabular osteotomy in patients fifty years of age or older. J Bone Joint Surg Am. 2010;92(1):31-41.[26] Yasunaga Y, Takahashi K, Ochi M, et al. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85-A(2):266-272.[27] Millis MB, Kain M, Sierra R, et al. Periacetabular osteotomy for acetabular dysplasia in patients older than 40 years: a preliminary study. Clin Orthop Relat Res. 2009;467(9): 2228-2234.[28] Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;(416):245-253.[29] Dora C, Mascard E, Mladenov K, et al. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop B. 2002; 11(1):34-40.[30] Dora C, Bühler M, Stover MD, et al. Morphologic characteristics of acetabular dysplasia in proximal femoral focal deficiency. J Pediatr Orthop B. 2004;13(2):81-87.[31] Dora C, Zurbach J, Hersche O, et al. Pathomorphologic characteristics of posttraumatic acetabular dysplasia. J Orthop Trauma. 2000;14(7):483-489.[32] Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;(363):93-99.[33] Clohisy JC, St John LC, Nunley RM, et al. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009;467(9):2221-2227.[34] Thawrani D, Sucato DJ, Podeszwa DA, et al. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg Am. 2010;92(8): 1707-1714.[35] Ziebarth K, Balakumar J, Domayer S, et al. Bernese periacetabular osteotomy in males: is there an increased risk of femoroacetabular impingement (FAI) after Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2011; 469(2):447-453.[36] Dorrell JH, Catterall A. The torn acetabular labrum. J Bone Joint Surg Br. 1986;68(3):400-403.[37] Leunig M, Werlen S, Ungersböck A, et al. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79(2):230-234.[38] Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423-429.[39] Leunig M, Podeszwa D, Beck M, et al. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;(418):74-80.[40] Hempfing A, Leunig M, Nötzli HP, et al. Acetabular blood flow during Bernese periacetabular osteotomy: an intraoperative study using laser Doppler flowmetry. J Orthop Res. 2003; 21(6): 1145-1150.[41] Langlotz F, Stucki M, Bächler R, et al. The first twelve cases of computer assisted periacetabular osteotomy. Comput Aided Surg. 1997;2(6):317-326.[42] Suh DH, Lee DH, Jeong WK, et al. Virtual Bernese osteotomy using three-dimensional computed tomography in hip dysplasia. Arch Orthop Trauma Surg. 2012;132(4):447-454. [43] Troelsen A, Søballe K. Advances in PAO surgery: the minimally invasive approach. Femoroacetabular Impingement. 2012:189-199. |
| [1] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [2] | Chen Lu, Zhang Jianguang, Deng Changgong, Yan Caiping, Zhang Wei, Zhang Yuan. Finite element analysis of locking screw assisted acetabular cup fixation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 356-361. |
| [3] | Fan Yinuo, Guan Zhiying, Li Weifeng, Chen Lixin, Wei Qiushi, He Wei, Chen Zhenqiu. Research status and development trend of bibliometrics and visualization analysis in the assessment of femoroacetabular impingement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 414-419. |
| [4] | Lin Tianye, Yang Peng, Xiong Binglang, He Xiaoming, Yan Xinhao, Zhang Jin, He Wei, Wei Qiushi . Comparison of preoperative three-dimensional reconstruction simulation and intraoperative drawing of femoral osteotomy to measure rotation angle in vitro [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3349-3353. |
| [5] | Huang Zeling, Shi Shanni, He Junjun, Gao Hongjian, Ge Haiya, Hong Zhenqiang. Meta-analysis of safety and effectiveness of proximal fibular osteotomy and high tibial osteotomy in the treatment of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2945-2952. |
| [6] | Liu Yongyu, Xu Jingli, Lin Tianye, Wu Feng, Shen Chulong, Xiong Binglang, Zou Qizhao, Lai Qizhong, Zhang Qingwen . Medium-and long-term follow-up of Salter pelvic osteotomy and implant fixation for children with developmental hip dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2380-2384. |
| [7] | Yang Youwei, Feng Wei . Quadrilateral plate fractures: research progress of implant treatment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2416-2422. |
| [8] | Ma Zhen, Liang Da, Wu Xiaolin, Zhong Wei . Safety evaluation of tranexamic acid in reducing perioperative blood loss in high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1847-1852. |
| [9] | Wang Debin, Bi Zhenggang. Optimization application for internal fixation strategy and three-dimensional printing technique of posterolateral tibial plateau fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1904-1910. |
| [10] | Wang Wencheng, Zhang Xingfei, Xu Yajun. Application of digital technology in the treatment of hallux valgus [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1911-1916. |
| [11] | Wang Hongshu, Han Shen, Liu Zu, Li Xiaofang, Zhong Chongbin, Li Lifeng, Li Yaxiong, Jiang Lihong. Transcription factor NKX2-5: molecular structure and biological function in regulating cardiovascular precursor cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(1): 108-115. |
| [12] | Li Guijun, Huang Kai, An Jinyu, Zhang Lei, Gao Libo, Gao Lei, Wu Yixiong, Lu Jiajun. New application of Endobutton suspension plate in hallux valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1365-1370. |
| [13] | Deng Biyong, Deng Bixiang. Differences in relative parameters of acetabulum in hip arthroplasty between CT horizontal plane and CT true pelvic plane [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1405-1409. |
| [14] |
Xie Fei, Li Yanle, Lin Xinxiao, Hu Haiwei, Sang Zhicheng, Sun Yongsheng, Jiang Kewei, Cheng Ying, Wen Guannan, Wen Jianmin, Sun Weidong.
Mechanism underlying mechanical stress regulating fibroblasts-derived
exosomes at the osteotomized end following hallux valgus correction |
| [15] | Wu Ronghai, Zhou Junde, Chen Peiyou, Yuan Liyi, Huang Junlin, Liang Zeqian, Wang Huimin. Meta-analysis of 3D printing-assisted posterior osteotomy for spinal deformity [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5880-5885. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||