Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (22): 3463-3468.doi: 10.3969/j.issn.2095-4344.1270
Previous Articles Next Articles
Bone grafting with recombinant human bone morphogenetic protein-2 or autologous platelet-rich plasma versus simple bone grafting for repair of bone defects
- First Department of Orthopedics, First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China
-
Received:2019-03-25 -
Contact:Zhou Qishi, Professor, First Department of Orthopedics, First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
About author:Li Shuyuan, Master candidate, First Department of Orthopedics, First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81674001 (to ZQS)
CLC Number:
Cite this article
Li Shuyuan, Zhou Qishi, Li Yue, Chen Chao, Chen Jiaqi, Zhou Hongliang, Yang Jiabao. Bone grafting with recombinant human bone morphogenetic protein-2 or autologous platelet-rich plasma versus simple bone grafting for repair of bone defects[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(22): 3463-3468.
share this article
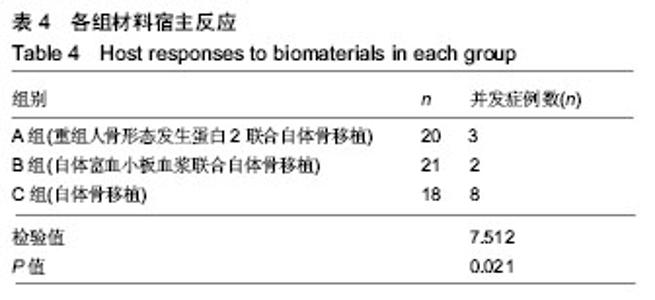
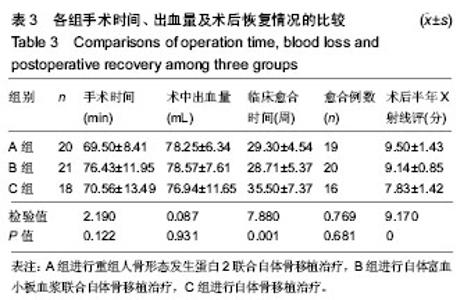
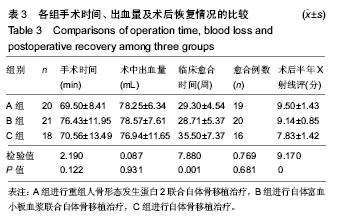
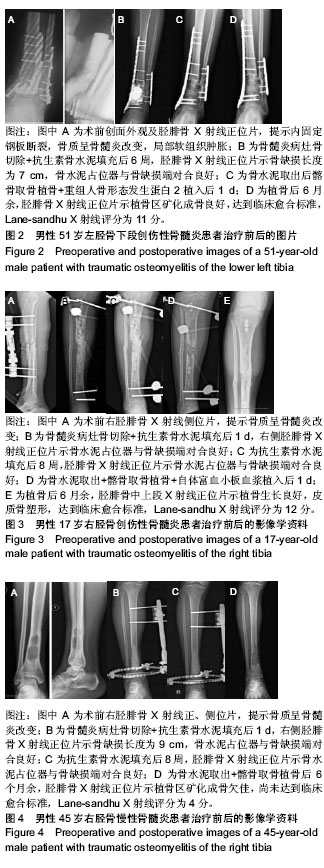
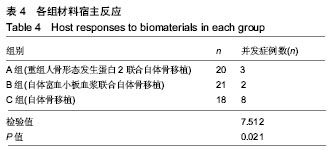
2.5 各组植骨区骨愈合效果的比较 从术后影像学结果评估,A组骨临床愈合时间为16-40周,B组为14-50周,C组为28-52周,A、B组骨临床愈合时间短于C组(P < 0.05)。A、B、C 组术后1年骨临床愈合例数分别为19,20,16例,3组比较差异无显著性意义(P > 0.05)。3组术后半年骨痂Lane-sandhu X射线评分比较差异有显著性意义(P < 0.05),见表3。 2.6 各组材料宿主反应 ①A组2例在植骨后出现深部感染,1例因感染累及胫骨关节面且周围软组织条件较差,后期行截肢手术,另1例改行骨搬运术后愈合;1例出现植骨后骨质吸收,经再次植骨后好转;该组使用重组人骨形态发生蛋白后未发现异位骨化、过度炎症反应等并发症;②B组1例出现深部感染,因感染严重后期行截肢手术,1例遗留膝关节僵硬伴中度疼痛,经麻醉下手法松解后好转;③C组4例在植骨后出现感染,其中1例为皮瓣周围的浅表感染、3例为深部感染,浅表感染经创面清创联合多次负压封闭引流术后感染控制,皮瓣愈合,3例深部感染中1例经再次清除病灶骨,改行Ilizarov骨搬运术后实现骨愈合,另外2例因深部感染未能控制,后期行截肢手术;3例在植骨后出现骨质吸收、延迟愈合,再次植骨后骨质愈合;1例遗留膝关节僵硬伴肌肉萎缩,经麻醉下手法松解和后期功能锻炼后关节活动度改善。A、B组并发症发生例数较C组更少(P < 0.05),见表4。"
| [1]赵御森,王海波,孟宪勇,等.组织工程骨修复超临界骨缺损研究进展[J].河北北方学院学报,2013,29(1):95.[2]Fishero BA,Kohli N,Das A,et al.Current concepts of bone tissue engineering for craniofacial bone defect repair.Craniomaxillofac Trauma Reconstr.2015;8(1):23-30.[3]Jeong SY, Hong JU, Song JM,et al. Combined effect of recombinant human bone morphogenetic protein-2 and low level laser irradiation on bisphosphonate-treated osteoblasts.J Korean Assoc Oral Maxillofac Surg.2018;44:259-268.[4]Bhujbal R,A Malik N,Kumar N,et al. Comparative evaluation of platelet rich plasma in socket healing and bone regeneration after surgical removal of impacted mandibular third molars. J Dent Res Dent Clin Dent Prospects.2018;12(3):153-158.[5]Cheng ZA,Alba-Perez A,Gonzalez-Garcia C,et al.Nanoscale Coatings for Ultralow Dose BMP-2-Driven Regeneration of Critical-Sized Bone Defects.Adv Sci.2019;6(2):1-12.[6]王腾飞,宋兴华,麦麦提艾力•阿不力克木,等.脂肪干细胞与羟基磷灰石/ β-磷酸三钙复合体修复兔椎体缺损[J].山东医药, 2018, 22(13):2081-2086.[7]Masquelet AC,Kishi T,Benko PE.Very long-term results of post-traumatic bone defect reconstruction by the induced membrane technique.Orthop Traumatol Surg Res. 2019; 105(1):159-166.[8]Masquelet AC.Induced membrane technique:pearls and pitfalls.J Orthop Trauma.2017;31 (Suppl 5):S36-S38.[9]Ronga M,Cherubino M,Corona K,et al.Induced membrane technique for the treatment of severe acute tibial bone loss: preliminary experience at medium-term follow-up.Int Orthop. 2019;43(1):209-215. [10]Akgun U,Canbek U,Aydogan NH,et al.Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury.2018; 49(3):738.[11]Christou C,Oliver RA,Yu Y,et al.The Masquelet technique for membrane induction and the healing of ovine critical sized segmental defects.PLoS One.2014;9(12): e114122.[12]McBride-Gagyi S,Toth Z,Kim D,et al.Altering spacer material affects bone regeneration in the Masquelet Technique in a Rat Femoral Defect.J Orthop Res.2018. doi: 10.1002/jor.23866. [Epub ahead of print][13]Gaio N,Martino A,Toth Z,et al.Masquelet technique: The effect of altering implant material and topography on membrane matrix composition, mechanical and barrier properties in a rat defect model. J Biomech.2018;72:53-62.[14]Aurégan JC,Bégué T,Rigoulot G,et al.Success rate and risk factors of failure of the induced membrane technique in children: a systematic review.Injury.2016;6(16):S62-S67.[15]Morelli I,Drago L,George DA,et al.Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. 2016; 47(6):S68-S76.[16]Ruehle MA,Krishnan L,Vantucci CE,et al.Effects of BMP-2 dose and delivery of microvascular fragments on healing of bone defects with concomitant volumetric muscle loss.J Orthop Res. 2019;37(3):553-561. [17]Kim S,Lee S,Kim K.Bone Tissue Engineering Strategies in Co-Delivery of Bone Morphogenetic Protein-2 and Biochemical Signaling Factors.Adv Exp Med Biol. 2018;1078:233-244.[18]Park J,Kim S,Kim K.Bone morphogenetic protein-2 associated multiple growth factor delivery for bone tissue regeneration.J Pharm Investig.2018;48(2):187-197.[19]Gonzaga MG,Dos Santos Kotake BG,Figueiredo FAT,et al. Effectiveness of rhBMP-2 association to autogenous, allogeneic, and heterologous bone grafts.Microsc Res Tech.2019.doi: 10.1002/jemt.23215. [Epub ahead of print].[20]Ishida W,Ramhmdani S,Xia Y,et al.Use of Recombinant Human Bone Morphogenetic Protein-2 at the C1-C2 Lateral Articulation without Posterior Structural Bone Graft in Posterior Atlantoaxial Fusion in Adult Patients.World Neurosurg. 2019;123:e69-e76.[21]Grey ZJ,Howie RN,Durham EL,et al.Sub-clinical dose of bone morphogenetic protein-2 does not precipitate rampant, sustained inflammatory response in bone wound healing. Wound Repair Regen. 2019. doi: 10.1111/wrr.12710.[Epub ahead of print].[22]Kizilda? A,Çiçek Y,Arabaci T,et al.The effect of leukocyte-platelet-rich fibrin on bone morphogenetic protein-2 and insulin-like growth factor-1 levels in patients with chronic periodontitis: a randomized split mouth clinical trail.Growth Factors.2019;9:239-245.[23]Hu J,Zeng Y,Shen C,et al.Mechanism of platelet-rich plasma in promoting bone defect repair. J Biol Regul Homeost Agents. 2019;33(1):97-103.[24]Yamada Y,Hara K,Nakamura S,et al. Minimally invasive approach with tissue engineering for severe alveolar bone atrophy case.Int J Oral Maxillofac Surg.2013;42:260-263.[25]Li H,Li B.PRP as a new approach to prevent infection: preparation and in vitro antimicrobial properties of PRP.J Vis Exp.2013;(74).doi: 10.3791/50351.[26]郭瑛,贾连顺,黄智.自体富血小板血浆在脊柱外科治疗中的应用[J].中国组织工程研究,2017,21(27):4403-4408.[27]Caplan AI,Sorrell JM.The MSC curtain that stops the immune system.Immunol Lett.2015;168:136-139.[28]Cheng A,Krishnan L,Pradhan P,et al.Impaired bone healing following treatment of established nonunion correlates with serum cytokine expression.J Orthop Res.2018;27:299-307.[29]唐勇,叶记超,胡旭民,等.基因重组人骨形态发生蛋白-2联合自体骨椎间打压植骨在腰椎融合术中的应用研究[J].中华骨与关节外科杂志,2018,9(11):664-667.[30]Cheng A,Krishnan L,Tran L,et al.The Effects of Age and Dose on Gene Expression and Segmental Bone Defect Repair Following BMP-2 Delivery.JBMR Plus.2019;3(2): e10068. |
| [1] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| [2] | Jiang Hongying, Zhu Liang, Yu Xi, Huang Jing, Xiang Xiaona, Lan Zhengyan, He Hongchen. Effect of platelet-rich plasma on pressure ulcers after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1149-1153. |
| [3] | Wu Xun, Meng Juanhong, Zhang Jianyun, Wang Liang. Concentrated growth factors in the repair of a full-thickness condylar cartilage defect in a rabbit [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1166-1171. |
| [4] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [5] | Li Cai, Zhao Ting, Tan Ge, Zheng Yulin, Zhang Ruonan, Wu Yan, Tang Junming. Platelet-derived growth factor-BB promotes proliferation, differentiation and migration of skeletal muscle myoblast [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1050-1055. |
| [6] | Liu Lihua, Sun Wei, Wang Yunting, Gao Fuqiang, Cheng Liming, Li Zirong, Wang Jiangning. Type L1 steroid-induced osteonecrosis of the femoral head through femoral head and neck junction decompression by fenestration: a single-center prospective clinical study [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 906-911. |
| [7] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [8] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [9] | Zhang Bin, Sun Lihua, Zhang Junhua, Liu Yusan, Cui Caiyun. A modified flap immediate implant is beneficial to soft tissue reconstruction in maxillary aesthetic area [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 707-712. |
| [10] | Luo Xuanxiang, Jing Li, Pan Bin, Feng Hu. Effect of mecobalamine combined with mouse nerve growth factor on nerve function recovery after cervical spondylotic myelopathy surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 719-722. |
| [11] | Nie Huijuan, Huang Zhichun. The role of Hedgehog signaling pathway in transforming growth factor beta1-induced myofibroblast transdifferentiation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 754-760. |
| [12] | Deng Zhenhan, Huang Yong, Xiao Lulu, Chen Yulin, Zhu Weimin, Lu Wei, Wang Daping. Role and application of bone morphogenetic proteins in articular cartilage regeneration [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 798-806. |
| [13] | Li Chenjie, Lü Linwei, Song Yang, Liu Jingna, Zhang Chunqiu. Measurement and statistical analysis of trabecular morphological parameters of titanium alloy peri-prosthesis under preload [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 516-520. |
| [14] | Liu Liu, Zhou Qingzhu, Gong Zhuo, Liu Boyan, Yang Bin, Zhao Xian. Characteristics and manufacturing techniques of collagen/inorganic materials for constructing tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 607-613. |
| [15] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||