Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (3): 586-595.doi: 10.12307/2025.865
Previous Articles Next Articles
Effects of three internal fixation techniques on biomechanics of adjacent segment degeneration in lumbar interbody fusion
Abudusalamu·Tuoheti1, 2, Xiao Yang1, Wang Yixi1, Musitapa·Mijiti3, Chen Qihao1, Maimaitiming·Saiyiti4, Guo Hailong1, Paerhati·Rexiti1, 5
- 1Department of Minimally Invasive Spine Surgery and Precision Orthopedics, 3Department of Rehabilitation Medicine, 4Department of Microreconstructive Surgery, First Affiliated Hospital of Xinjiang Medical University, Urumqi 830000, Xinjiang Uygur Autonomous Region, China; 2Department of Spine and Traumatology, The Second People's Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830002, Xinjiang Uygur Autonomous Region, China; 5Key Laboratory of High Incidence Diseases Research of Ministry of Education (Xinjiang Medical University), Urumqi 830000, Xinjiang Uygur Autonomous Region, China
-
Received:2024-07-22Accepted:2024-11-20Online:2026-01-28Published:2025-07-03 -
Contact:Paerhati·Rexiti, Chief physician, Professor, Doctoral and master’s supervisor, Department of Minimally Invasive Spine Surgery and Precision Orthopedics, First Affiliated Hospital of Xinjiang Medical University, Urumqi 830000, Xinjiang Uygur Autonomous Region, China; Key Laboratory of High Incidence Diseases Research of Ministry of Education (Xinjiang Medical University), Urumqi 830000, Xinjiang Uygur Autonomous Region, China -
About author:Abudusalamu•Tuoheti, Master candidate, Department of Minimally Invasive Spine Surgery and Precision Orthopedics, First Affiliated Hospital of Xinjiang Medical University, Urumqi 830000, Xinjiang Uygur Autonomous Region, China; Department of Spine and Traumatology, The Second People's Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830002, Xinjiang Uygur Autonomous Region, China -
Supported by:Outstanding Youth Science Fund of Xinjiang Uygur Autonomous Region, No. 2021D01E29 (to PR); “Tianshan Talents” Medical and Health High-level Talent Training Program Fund, No. TSYC202301B026 (to PR); Graduate Innovation Project Fund of Xinjiang Uygur Autonomous Region, No. XJ2024G158 (to AT)
CLC Number:
Cite this article
Abudusalamu·Tuoheti, Xiao Yang, Wang Yixi, Musitapa·Mijiti, Chen Qihao, Maimaitiming·Saiyiti, Guo Hailong, Paerhati·Rexiti. Effects of three internal fixation techniques on biomechanics of adjacent segment degeneration in lumbar interbody fusion[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 586-595.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
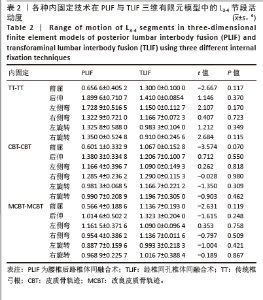
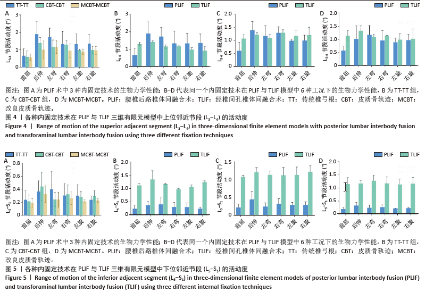
2.1 模型的有效性验证 在建立的有限元模型中生成了网格1、网格2、网格3等3种网格分辨率,并通过比较网格1与网格3、网格2与网格3之间von Mises应力的百分比差异,进行收敛性分析验证了网格2的可靠性[20]。随后模拟脊柱在前屈、后伸、左侧弯、右侧弯、左旋转和右旋转6种不同工况下,在400 N垂直向下压缩力和7.5 Nm扭矩作用下的邻近节段活动度。分析结果显示,完整模型的活动度与YAMAMOTO等[25]、SHIM等[26]、HUANG等[27]和LO等[28]的研究结果和变化趋势相似,进而验证了该有限元模型用于进一步生物力学分析的有效性和准确性,也与之前的研究结果相符[20]。 2.2 L3-L4节段活动度 TT-TT组在PLIF模型后伸时表现出了最高的L3-L4活动度,为(1.899 6±0.710 7)°,而在前屈时最低(0.656 6±0.405 2)°。在TLIF模型后伸时表现出了最高的L3-L4活动度,为(1.410 0±0.085 4)°,而在右旋转时最低(0.910 0± 0.245 6)°。CBT-CBT组在PLIF模型后伸时表现出了最高的L3-L4活动度,为(1.380 3±0.334 8)°,而在前屈时最低(0.601 1± 0.332 9)°。在TLIF模型右侧弯时表现出了最高的L3-L4活动度,为(1.290 0±0.115 3)°,而在前屈时最低(1.067 0±0.152 8)°。MCBT-MCBT组在PLIF模型左侧弯时表现出了最高的L3-L4活动度,为(1.161 5±0.371 6)°,而在前屈时最低(0.566 4±0.188 6)°。在TLIF模型后伸时表现出了最高的L3-L4活动度,为(1.323 3±0.204 0)°,而在左旋转时最低(0.993 3±0.218 3)°。见图4及表2。"

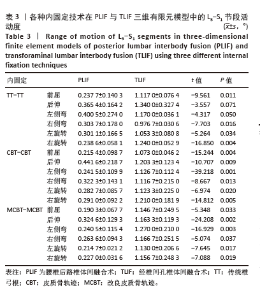
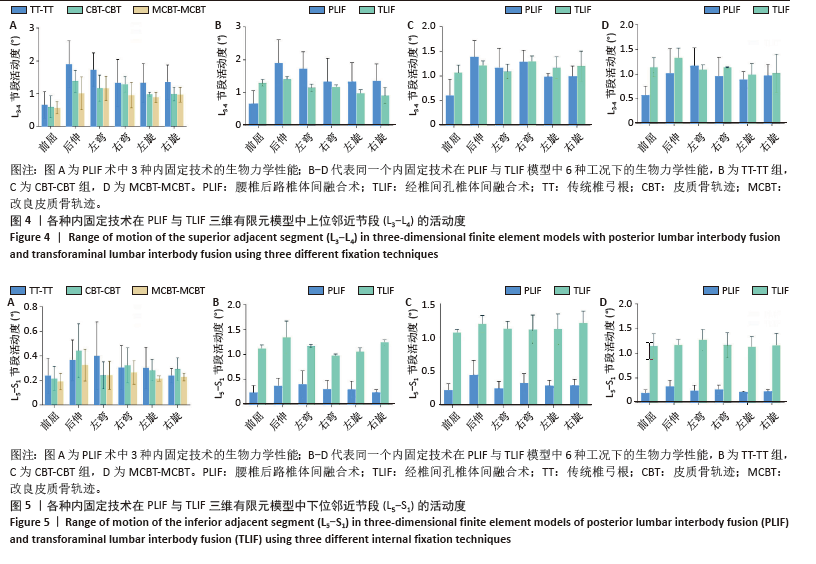
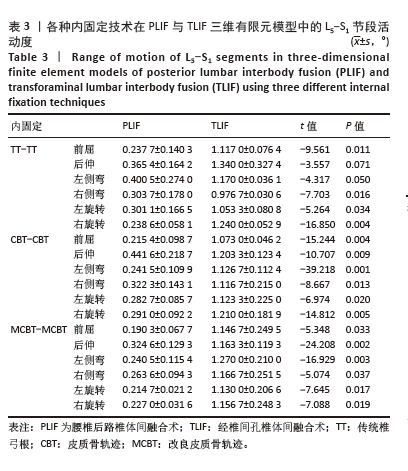
2.3 L5-S1节段活动度 TT-TT组在PLIF模型左侧弯时表现出了最高的L5-S1活动度,为(0.400 5±0.274 0)°,而在前屈时最低(0.237 7±0.140 3)°;在TLIF模型后伸时表现出了最高的L5-S1活动度,为(1.340 0±0.327 4)°,而在右侧弯时最低(0.976 7±0.030 6)°。CBT-CBT组在PLIF模型后伸时表现出了最高的L5-S1活动度,为(0.441 6±0.218 7)°,而在前屈时最低(0.215 4±0.098 7)°;在TLIF模型右旋转时表现出了最高的L5-S1活动度,为(1.210 0±0.181 9)°,而在前屈时最低(1.073 0±0.046 2)°。MCBT-MCBT组在PLIF模型后伸时表现出了最高的L5-S1活动度,为(0.324 6±0.129 3)°,而在前屈时最低(0.190 3±0.067 7)°;在TLIF模型左侧弯时表现出了最高的L5-S1活动度,为(1.270 0±0.210 0)°,而在左旋转时最低(1.130 0±0.206 6)°,见图5及表3。"
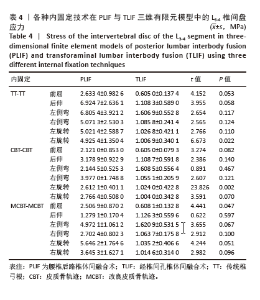
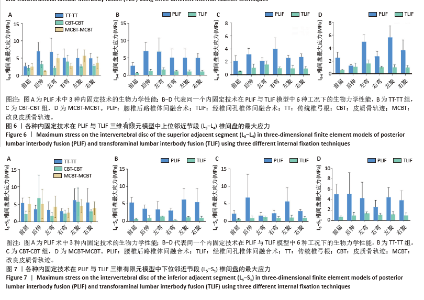
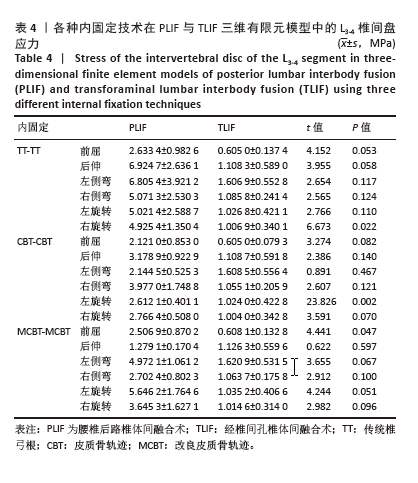
2.4 L3-L4节段椎间盘应力 TT-TT组在PLIF模型后伸时表现出了最大L3-L4椎间盘应力(6.924 7±2.636 1) MPa,而在前屈时最低(2.633 4±0.982 6) MPa。在TLIF模型左侧弯时表现出了最大L3-L4椎间盘应力(1.606 9±0.552 8) MPa,而在前屈时最低(0.605 0±0.137 4) MPa。CBT-CBT组在PLIF模型右侧弯时表现出了最大L3-L4椎间盘应力(3.977 0±1.748 8) MPa,而在前屈时最低(2.121 0±0.853 0) MPa。在TLIF模型左侧弯时表现出了最大L3-L4椎间盘应力(1.608 5±0.556 4) MPa,而在前屈时最低(0.605 0±0.079 3) MPa。MCBT-MCBT组在PLIF模型左旋转时表现出了最大L3-L4椎间盘应力(5.646 2±1.764 6) MPa,而在后伸时最低(1.279 1±0.170 4) MPa。在TLIF模型左侧弯时表现出了最大L3-L4椎间盘应力(1.620 9±0.531 5) MPa,而在前屈时最低(0.608 1±0.132 8) MPa,见图6及表4。"
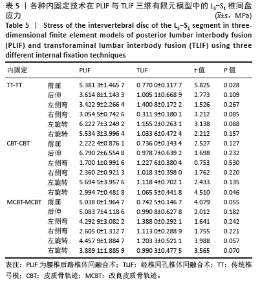
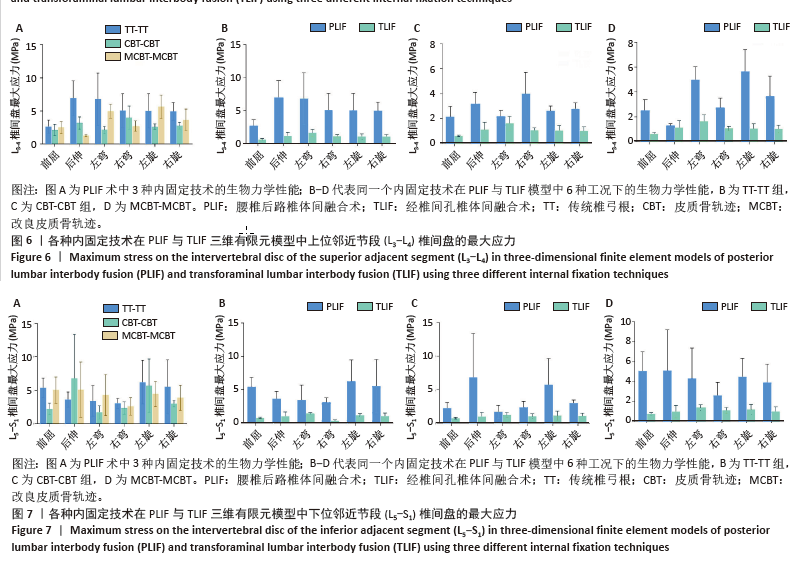
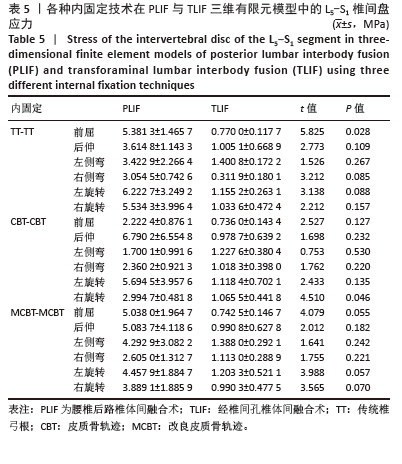
2.5 L5-S1节段椎间盘应力 TT-TT组在PLIF模型左旋转时表现出了最大L5-S1椎间盘应力,为(6.222 7±3.249 2) MPa,而在右侧弯时最低(3.054 5±0.742 6)MPa;在TLIF模型左侧弯时表现出了最大的L5-S1椎间盘应力,为(1.400 8±0.172 2)MPa,而在右侧弯时最低(0.311 9±0.180 1) MPa。CBT-CBT组在PLIF模型后伸时表现出了最大的L5-S1椎间盘应力,为(6.790 2±6.554 8) MPa,而在左侧弯时最低(1.700 1±0.991 6)MPa;在TLIF模型左侧弯时表现出了最大的L5-S1椎间盘应力,为(1.227 6±0.380 4) MPa,而在前屈时最低(0.736 0±0.143 4) MPa。MCBT-MCBT组在PLIF模型后伸时表现出了最大的L5-S1椎间盘应力,为(5.083 7±4.118 6) MPa,而在右侧弯时最低(2.605±1.312 7) MPa;在TLIF模型左侧弯时表现出了最大的L5-S1椎间盘应力(1.388±0.292 1) MPa,而在前屈时最低(0.742 5±0.146 7) MPa。见图7及表5。"
| [1] RAVINDRA VM, SENGLAUB SS, RATTANI A, et al. Degenerative Lumbar Spine Disease: Estimating Global Incidence and Worldwide Volume. Global Spine J. 2018;8(8):784-794. [2] PARK P, GARTON HJ, GALA VC, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004;29(17):1938-1944. [3] 宋佳伟, 杨永栋, 俞兴,等. Isobar EVO非融合动态固定治疗腰椎融合术后邻椎病的中期疗效[J]. 中国组织工程研究,2022,26(6): 908-913. [4] MIMURA T, TSUTSUMIMOTO T, YUI M, et al. Adjacent segment pathology following posterior lumbar interbody fusion for lumbar degenerative spondylolisthesis: a comparison between minimally invasive and conventional open approach. Spine J. 2021;21(8): 1297-1302. [5] CORIC D, BRANCH CL JR. Posterior lumbar interbody fusion in the treatment of symptomatic spinal stenosis. Neurosurg Focus. 1997;3(2):e5. [6] DE KUNDER SL, VAN KUIJK SMJ, RIJKERS K, et al. Transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) in lumbar spondylolisthesis: a systematic review and meta-analysis. Spine J. 2017;17(11):1712-1721. [7] CHEN M, CUI J, LIU Y, et al. Comparison of safety and efficacy of posterior lumbar interbody fusion (PLIF) and modified transforaminal lumbar interbody fusion (M-TLIF) in the treatment of single-segment lumbar degenerative diseases. J Orthop Surg Res. 2024;19(1):95. [8] MARAGKOS GA, ATESOK K, PAPAVASSILIOU E. Prognostic Factors for Adjacent Segment Disease After L4-L5 Lumbar Fusion. Neurosurgery. 2020;86(6):835-842. [9] LEE CW, YOON KJ, HA SS. Which Approach Is Advantageous to Preventing Development of Adjacent Segment Disease? Comparative Analysis of 3 Different Lumbar Interbody Fusion Techniques (ALIF, LLIF, and PLIF) in L4-5 Spondylolisthesis. World Neurosurg. 2017;105: 612-622. [10] DING H, HAI Y, LIU Y, et al. Cortical Trajectory Fixation Versus Traditional Pedicle-Screw Fixation in the Treatment of Lumbar Degenerative Patients with Osteoporosis: A Prospective Randomized Controlled Trial. Clin Interv Aging. 2022;17:175-184. [11] SANTONI BG, HYNES RA, MCGILVRAY KC, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366-373. [12] REXITI P, ABUDUREXITI T, ABUDUWALI N, et al. Measurement of lumbar isthmus parameters for novel starting points for cortical bone trajectory screws using computed radiography. Am J Transl Res. 2018;10(8): 2413-2423. [13] REXITI P, AIERKEN G, WANG S, et al. Anatomical research on strength of screw track fixation in novel cortical bone trajectory for osteoporosis lumbar spine. Am J Transl Res. 2019;11(11):6850-6859. [14] REXITI P, AIERKEN A, SADEER A, et al. Anatomy and Imaging Studies on Cortical Bone Screw Freehand Placement Applying Anatomical Targeting Technology. Orthop Surg. 2020;12(6):1954-1962. [15] KIAPOUR A, AMBATI D, HOY RW, et al. Effect of graded facetectomy on biomechanics of Dynesys dynamic stabilization system. Spine. 2012;37(10): E581-E589. [16] LU YM, HUTTON WC, GHARPURAY VM. Do bending, twisting, and diurnal fluid changes in the disc affect the propensity to prolapse? A viscoelastic finite element model. Spine. 1996;21(22):2570-2579. [17] NATARAJAN RN, WATANABE K, HASEGAWA K. Biomechanical analysis of a long-segment fusion in a lumbar spine-a finite element model study. J Biomech Eng. 2018;140(9):091011 [18] KIM HJ, CHUN HJ, LEE HM, et al. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J Off J North Am Spine Soc. 2013;13(10):1301-1308. [19] FAN W, GUO LX, ZHAO D. Stress analysis of the implants in transforaminal lumbar interbody fusion under static and vibration loadings: a comparison between pedicle screw fixation system with rigid and flexible rods. J Mater Sci Mater Med. 2019;30(10):118. [20] KAHAER A, ZHANG R, WANG Y, et al. Hybrid pedicle screw and modified cortical bone trajectory technique in transforaminal lumbar interbody fusion at L4-L5 segment: finite element analysis. BMC Musculoskelet Disord. 2023;24(1):288. [21] TUOHETI A, XIAO Y, WANG Y, et al. Biomechanical evaluation of modified and traditional cortical bone trajectory technique on adjacent segment degeneration in transforaminal lumbar interbody fusion-finite element analysis. BMC Musculoskelet Disord. 2024,25(1):7. [22] SANSUR CA, CAFFES NM, IBRAHIMI DM, et al. Biomechanical fixation properties of cortical versus transpedicular screws in the osteoporotic lumbar spine: an in vitro human cadaveric model. J Neurosurg Spine. 2016;25(4):467-476. [23] ROY-CAMILLE R, SAILLANT G, MAZEL C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop. 1986;203(203):7-17. [24] MATSUKAWA K, YATO Y, IMABAYASHI H, et al. Biomechanical evaluation of the fixation strength of lumbar pedicle screws using cortical bone trajectory: a finite element study. J Neurosurg Spine. 2015;23(4): 471-478. [25] YAMAMOTO I, PANJABI MM, CRISCO T, et al. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine. 1989;14(11):1256-1260. [26] SHIM CS, PARK SW, LEE SH, et al. Biomechanical evaluation of an interspinous stabilizing device. Locker Spine. 2008;33(22): E820-827. [27] HUANG YP, DU CF, CHENG CK, et al. Preserving posterior complex can prevent adjacent segment disease following posterior lumbar interbody fusion surgeries: a finite element analysis. PLoS ONE. 2016;11(11): e0166452. [28] LO HJ, CHEN HM, KUO YJ, et al. Effect of different designs of interspinous process devices on the instrumented and adjacent levels after double-level lumbar decompression surgery: A finite element analysis. PLoS ONE. 2020;15(12): e0244571. [29] HASHIMOTO K, AIZAWA T, KANNO H, et al. Adjacent segment degeneration after fusion spinal surgery: a systematic review. Int Orthop. 2019;43(4):987-993. [30] 张腾飞,王坤,朱彦谕,等.腰椎后路融合术后邻近节段退变相关危险因素的Meta分析[J].中国组织工程研究,2021,25(12): 1936-1943. [31] PAN A, HAI Y, YANG J, et al. Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J. 2016;25(5):1522-1532. [32] ROUSSEAU MA, LAZENNEC JY. Degenerative disease supra- and infra-jacent to fused lumbar and lumbo-sacral levels. Orthop Traumatol Surg Res. 2016;102(1Suppl): S1-S8. [33] 李大川,卢枭,徐广宇,等. 椎旁肌萎缩及关节突关节形态改变与腰椎融合术后邻近节段疾病的相关性[J]. 中华骨科杂志,2022, 42(19):1292-1300. [34] WILLBURGER RE, KRÄMER J, WIESE M. Surgical anatomy of the lumbar spine. Orthopade. 2005;34(10):970-975. [35] BANIEL J, FOSTER RS, DONOHUE JP. Surgical anatomy of the lumbar vessels: implications for retroperitoneal surgery. J Urol. 1995;153(5): 1422-1425. [36] KUMAR MN, BAKLANOV A, CHOPIN D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10(4):314-319. [37] 卢枭,邹飞,吕飞舟,等. 斜外侧腰椎间融合术中椎间融合器高度对邻近节段退变影响的三维有限元分析[J]. 中华骨科杂志,2022, 42(19):1301-1311. [38] LU X, LI D, WANG H, et al. Biomechanical effects of interbody cage height on adjacent segments in patients with lumbar degeneration: a 3D finite element study. J Orthop Surg Res. 2022;17(1):325. [39] LU X, ZOU F, LU F, et al. How to reconstruct the lordosis of cervical spine in patients with Hirayama disease? A finite element analysis of biomechanical changes focusing on adjacent segments after anterior cervical discectomy and fusion. J Orthop Surg Res. 2022; 17(1):101. [40] SAKAURA H, MIWA T, YAMASHITA T, et al. Cortical bone trajectory screw fixation versus traditional pedicle screw fixation for 2-level posterior lumbar interbody fusion: comparison of surgical outcomes for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2018;28(1):57-62. [41] LEE GW, SON JH, AHN MW, et al. The comparison of pedicle screw and cortical screw in posterior lumbar interbody fusion: a prospective randomized noninferiority trial. Spine J. 2015;15(7): 1519-1526. [42] HU Q, GAO X, LEVENE HB, et al. Influences of nutrition supply and pathways on the degenerative patterns in human intervertebral disc. Spine (Phila Pa 1976). 2016;41(7):568-576. [43] FUJIWARA S, OHNISHI Y, IWATSUKI K, et al. Cortical bone trajectory fixation cause low compression force in anterior vertebral column. N Am Spine Soc J. 2022;10:100113. [44] MAITIROUZI J, LUO H, ZHOU Z, et al. Finite element analysis of human lumbar vertebrae in internal fixation system model with different bone density trajectories. Int J Artif Organs. 2022;45(5):478-487. [45] 刘东山,王轶希,帕尔哈提·热西提. 腰椎融合术后邻近节段病的微创手术治疗进展[J]. 中华外科杂志,2023,61(8):722-727. |
| [1] | Wang Yalei, Wang Xuezhi, Zhou Tao, Shen Xinxin, Fang Ding, Chen Hongliang. Effect of sacroiliac joint ankylosis on outcomes of L5/S1 transforminal lumbar interbody fusion and lumbar sagittal parameters [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 634-641. |
| [2] | Yu Xinlin, Chen Huiyu, Wang Yingying, Guo Weizhong, Feng Bin Lin Chengshou, Lin Wang. Finite element analysis of internal fixation with new retrograde intramedullary nail on lateral femur condyle for distal type A2 femur fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 546-552. |
| [3] | Zhao Jingang, Liu Liping, Chen Jianwei, . Finite element analysis comparing lumbar fusion and artificial intervertebral disc replacement [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 553-560. |
| [4] | Wang Meng, Lu Tan, Li Minjie, Liu Zhicheng, Guo Xiaoyong. Finite element analysis of stress distribution of anchors at different implantation depths under different bone density conditions in rotator cuff tears [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 561-569. |
| [5] | Ma Jingbo, Yang Guangnan, Liu Jiang, Jiang Qiang, Zhang Hanshuo, Han Jiaheng, Ding Yu. Endoscopic lumbar canal decompression for upper lumbar spinal stenosis: a comparison of biomechanical stability of three surgical models [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 577-585. |
| [6] | Shang Depeng, Wei Haiyu, Yang Fan. Finite element analysis for three different types of internal screw fixation in treatment of severe lumbar 1 vertebral body fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 537-545. |
| [7] | Cheng Yanan, Yu Jiazhi, Liu Yinchang, Wu Jie, Yu Tong, Wang Lu, Li Xiaoguang. Three-dimensional finite element analysis of molar distalization with clear aligners with different thicknesses and edges [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 310-318. |
| [8] | Kang Zirui, Wu Yang, Song Hailong, Yang Qiaoyun, Zang Lixiang, Xu Dongliang. Finite element analysis of implants with different crown-to-implant ratios under different bone conditions [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 319-328. |
| [9] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [10] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [11] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [12] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [13] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [14] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [15] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||