Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (27): 5883-5889.doi: 10.12307/2025.811
Previous Articles Next Articles
Application of 3D printing technology in traumatic fractures
Lian Zeshuang1, Xu Qiang1, Wang Aoting1, Li Ding1, 2, Qin Jialin1, 2, Wang Junfang1, 2
- 1Nanjing Medical University, Nanjing 211166, Jiangsu Province, China; 2Department of Orthopedics, Wuxi People’s Hospital Affiliated to Nanjing Medical University, Wuxi 214023, Jiangsu Province, China
-
Received:2024-05-22Accepted:2024-07-15Online:2025-09-28Published:2025-03-06 -
Contact:Wang Junfang, MD, Chief physician, Master’s supervisor, Nanjing Medical University, Nanjing 211166, Jiangsu Province, China; Department of Orthopedics, Wuxi People’s Hospital Affiliated to Nanjing Medical University, Wuxi 214023, Jiangsu Province, China -
About author:Lian Zeshuang, MS, Nanjing Medical University, Nanjing 211166, Jiangsu Province, China -
Supported by:Wuxi Municipal Health Commission Young and Middle-aged Talents Funding Program, No. BJ2023015 (to WJF)
CLC Number:
Cite this article
Lian Zeshuang, Xu Qiang, Wang Aoting, Li Ding, Qin Jialin, Wang Junfang. Application of 3D printing technology in traumatic fractures[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5883-5889.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
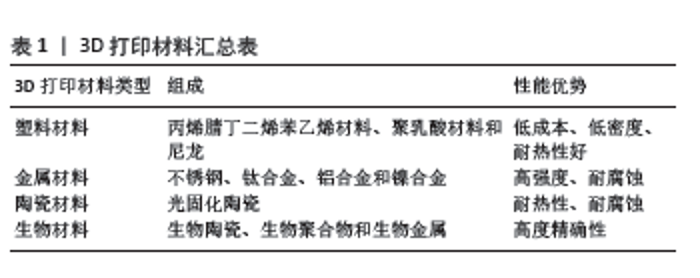
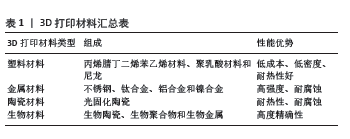
2.1 骨折损伤机制及主流治疗方案 创伤性骨折是高能量冲击等机械因素在短时间内造成的伴软组织、血管神经和内脏损伤的骨折现象,患者临床表现为明显疼痛、肿胀畸形和局部活动受限等症状,创伤严重时可造成休克死亡[5-6]。当前临床治疗创伤性四肢骨折的方案,常由骨科医师依据多变临床经验、解剖学知识、手术路径掌握程度和自身空间立体构想能力进行规划制定,早期识别骨折相关力学模式以有效治疗方案恢复骨折和获取骨折修复稳定性[7],结合X射线片、CT和MRI等影像资料的二维或三维平面图像,在屏幕中还原骨折虚拟成像情况[8-9]。但此类方案通常因局部解剖复杂和空间构想能力欠缺等因素导致难以真实还原骨折原貌,对创伤性骨折固定治疗造成不利影响[10-11]。因此,探究更为有效的骨折治疗方案,精准了解损伤类型及周围解剖关系,科学、直观和精确地重建骨折模型,已成为当前创伤性骨折治疗研究领域的热点问题。 2.2 3D打印技术基本工作原理和打印技术及材料 3D打印技术是以数字模型数据和计算机辅助设计软件的三维设计重建等功能为基础,运用黏合材料逐层打印目标层面得到预期实物模型的新型快速成型技术,融合了数据处理、计算机统计分析、打印成型和构建模型等技术的优势[12-14]。3D打印技术的基本工作原理是通过分层构建以数字设计模型为蓝本,逐层叠加打印材料逐渐组装制造出形状复杂和结构独特的实体产品,包含模型创建、切片、逐层堆积、层间黏合和重复堆积等操作步骤[15-18]。在打印技术方面,目前应用广泛的技术包含熔融沉积建模、光固化、选择性激光烧结及粉末热熔等,各种技术均具有独特的优点和限制,需综合考虑精度、材料特性、成本和打印物体设计需求等因素,应用于医疗保健、制造业、航空航天和建筑等领域[19]。在打印材料方面,3D打印通常依据材料的化学成分和物理性质分为金属、陶瓷、塑料和生物材料等类型[20-22],见表1。"
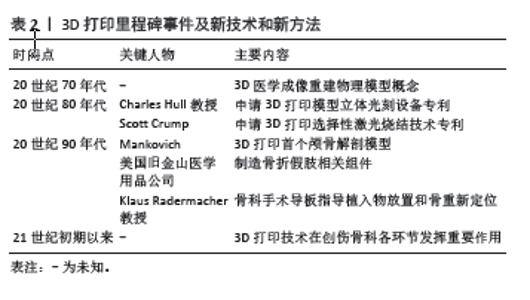
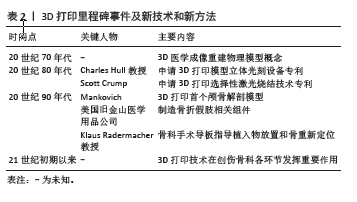
2.3 3D打印技术在创伤性骨折领域技术和方法的发展历史 3D打印技术隶属于数字骨科,是结合计算机数字技术和骨科诊疗实现精准外科治疗的新兴交叉学科,解决了传统创伤骨科的诸多难题[23]。在过去的几十年里,3D打印技术在医药和航空航天工业、汽车工业、厨具制造行业等多个领域获得了长足的发展。20世纪70年代,3D医学成像重建物理模型概念首次提出,20世纪80年代中期Charles Hull教授和Scott Crump先后申请了3D打印模型的立体光刻设备和选择性激光烧结技术的专利,并发明了首台3D打印机和商用3D打印机,开创了3D打印的新时代[24]。20世纪90年代,Mankovich依据CT扫描数据以立体光刻设备制作了首个颅骨解剖模型,这是3D打印技术在医学领域的首次应用。随后,美国旧金山医学用品公司开始为骨折患者制造假肢相关组件。德国教授Klaus Radermacher引入计算机辅助骨科手术导板概念,将其应用于指导植入物放置和骨重新定位,为实现植入物或假体的准确放置,手术导板的使用实现了由术前计划到术前模拟实际手术部位的飞跃,有效提高了骨折修复手术的精确度和安全性[25]。21世纪初期以来,计算机3D打印技术在骨科应用方面取得了重大进展,随着骨科椎弓根螺钉放置指南的制定颁布,3D打印技术在创伤骨科的各个环节发挥重要作用,实现了创伤性骨折治疗精准、智能和微创的目标[26]。见表2。"
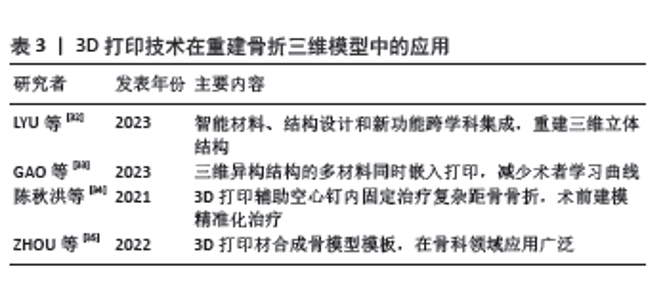
2.4 3D打印技术在创伤性骨折中的应用情况 3D打印技术在医疗领域中应用分为快速成型、辅助工具制作、植入材料制造和生物活体及组织工程制造等,可利用3D打印技术设计和制造特定的骨科植入体、固定支具和骨骼支架等仿生器官,还可设计制造定制支撑器件和外科手术工具等医疗器械[27]。近年来,随着数字医学和影像成像技术在相关领域的快速发展,3D打印技术在复杂骨折的诊断、术前规划、骨科实体模型、导航模板设计和骨缺损修复方面发挥了显著的优势,为骨外科领域疑难骨折手术方案制定提供了新的思路,展示了巨大的应用前景。 2.4.1 3D打印技术在创伤性骨折疾病诊断和术前规划中的应用 在创伤骨折临床诊断流程中,通常会碰到寻找骨折线的走向、确认骨折块方位、确认固定计划、螺钉与钢板位置的调节等难题。复杂股骨远端骨折中股骨远端的解剖结构发生严重变化,传统依靠X射线片、CT等辅助检查资料判断患者股骨远端骨折分型制定手术方案的方法逐渐显现出诸多弊病,难以满足当前临床精准医疗的需求[28]。3D打印技术对打印机所获CT三维重建扫描数据进行运算分析,制作出与患肢等比例的股骨远端骨折3D模型,以细致观察、深入理解骨折的解剖特点,准确判断骨折分型,可为最佳手术方案的制定提供指导[29]。利用3D模型进行模拟验证,对手术过程进行预演,熟练掌握术中操作技巧,能够确保减少术中出血量、缩短手术操作时间。全彩3D打印模型在手术计划流程中可以清楚地呈现骨块的移位与压缩状况,辅助医师更加迅速清楚地厘清复位思路[30]。 2.4.2 3D打印技术在重建骨折三维模型中的应用 3D打印技术可结合影像技术通过三维编辑功能对骨折块分离、旋转和移动等进行虚拟复位和模拟手术,精准重建骨折的三维模型[31]。与以往屏幕中虚拟3D图像比较,3D或4D打印技术与骨科模型导板设计结合可直观显示相关骨骼解剖结构及其与周围软组织的关系,辅助医护人员直观重建骨折三维立体结构和准确判断骨折分型,在术前根据骨折模型制定详细的手术规划并进行反复推演,以此设计最佳手术方案,并帮助患者全面详细了解骨折及组织损伤情况[32]。依据3D打印骨折三维模型预设手术方案,提前定位复位点和置入螺钉或钢板,提前进行手术演练,以3D打印导板辅助手术操作,可有效降低对术者手术经验和技术能力的依赖,减少术者学习曲线,在推进创伤性骨折微创治疗方面优势显著[33]。据陈秋洪等[34]文献报道,利用3D打印技术对复杂距骨骨折、骨盆骨折等进行术前建模,可达到精准化及个体化治疗的目的。另有研究显示,以实际尺寸3D打印的正常骨模型为模板,选择与骨贴合最佳的解剖型接骨板并提前模拟其具体放置位置和螺钉运动轨迹等术前模拟和手术方案设计,在骨科领域展现了良好的应用价值[35]。见表3。"
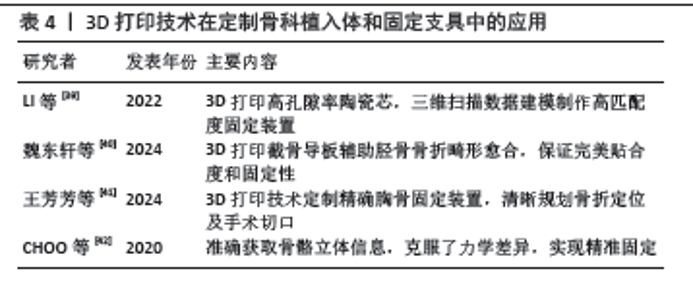
2.4.3 3D打印技术在定制骨科植入体中的应用 骨科植入物领域是3D打印制造行业最成功的案例之一,该领域通常应用金属、陶瓷或特殊聚合物以激光粉末床熔融、选择性激光熔融或电子束熔融技术制造复杂表面结构的植入物,在骨愈合评估、膝关节受力分析、脊柱融合监测和髋关节假体松动监测中具有较好的应用价值[36]。在创伤性骨折手术过程中,按数字模型文件以3D打印技术逐层打印粉末金属和塑料等可黏合材料的医疗植入物,可显著提高固定装置的准确性和稳定性,在改善手术效果和提高固定成功率方面优势显著[37]。3D打印技术可制作辅助骨折复位、置入内固定接骨板或螺钉的手术导航模板,通过定制精确的骨固定装置,使骨折的定位以及手术切口规划更加明确清晰。通过3D打印模型充分了解骨折情况,依据术前设计的导航模板辅助手术,可帮助骨折端精准复位和螺钉准确置入,使手术操作更加准确[38]。 2.4.4 3D打印技术在定制固定支具和假肢中的应用 传统骨科固定支具通常不能与个体完美匹配,临床工作中也常会遇到内固定物产品和假肢与骨折部位解剖形态匹配不良的场景,导致无法满足患者需求,对康复造成不利影响。3D打印技术结合创伤性骨折患者影像学特征和治疗需求,以三维扫描数据建模制作高匹配度的固定装置,保证完美的贴合度和固定性[39-40]。王芳芳等[41]研究发现,以3D打印技术定制精确的胸骨固定装置,可使胸骨及肋骨骨折的定位以及手术切口规划更加明确清晰。CHOO等[42] 的文献显示,由计算机编程设计的3D打印固定装置可准确获取患者骨骼尺寸位置等立体信息,克服了传统固定装置精准度欠缺导致的力学差异,具有精准固定的优势。见表4。 2.4.5 3D打印技术在手术导板制作中应用 3D打印手术导板是用于指导放置螺钉等内固定物、帮助骨重新定位和帮助确定截骨范围的工具,外科医生可在手术导板帮助下轻松确定螺钉路径的方向和深度,选择截骨角度和范围,提高手术精度、安全性和可靠性[43-45]。此外,3D打印手术导板还可简化手术步骤、缩短医师学习曲线、加速中青年医师的成长,越来越受到临床医生的关注。手术导航实物模板可帮助骨折精准复位,使辅助器械或各种植入物达到预定位置,有效降低置钉方向错误率及提高手术操作的准确性,是临床常用的手术指导辅助工具[46-47]。传统的手术导板制作通常采用机械加工和手工制作等方式,制作周期长,且制作成本较高,限制了其临床应用。3D打印技术在手术导板制作中具有较好的应用效果,可制作传统方法难以加工的复杂形状和结构,兼具响应速度快、定制化、适用性广和低成本等优势,满足了当前手术高精度的要求[48]。在制作3D打印手术导板时,常通过医学图像处理软件处理患者CT、MRI等医学影像数据后生成三维数字模型,以3D打印技术将该模型转化为实体模型,制作个体化的手术导板[49]。3D打印骨科手术导板制作的临床应用包含置钉导板、截骨导板和其他系列导板。以往骨科医生通常使用徒手技术或术中X射线图像选择创伤性骨折手术螺钉的轨迹,但较易引起脊髓和椎动脉损伤,增加了患者和术者的辐射暴露风险。经皮模板3D打印置钉导板可指导术中精确放置螺钉,避免重要血管和神经的损伤,克服了空间结构的影响,提高了置钉准确性[50-51]。3D打印截骨导板在创伤骨折术前准确规划和设计截骨范围至关重要,可避免损伤相邻神经和血管,维持截骨后的平衡性,使截骨手术进入数字化阶段。在创伤骨科领域,3D打印手术导板可指导骨折复位和关节置换等手术操作,为患者提供更为精准的手术治疗[52-53]。 2.4.6 3D打印技术在骨缺损修复中的应用 创伤骨折中骨缺损多由严重创伤、感染灶清除、畸形矫正和翻修手术引起,是造成骨不愈合和肢体畸形的重要原因,增加家庭与社会的经济负担[54]。3D打印假体包含非多孔、全多孔、部分多孔、框架、笼架和铰链等结构,适用于重建或修复骨缺损。3D生物打印技术可实现细胞精准的三维空间调控,将血管网络打印进仿骨支架的内部。在骨缺损的修复中经常需要使用到植入物,传统骨科植入物的尺寸和形状为固定形式,术中需采用骨锉刀修整宿主骨,使假体和内植物形状和尺寸相匹配[55]。3D打印可为患者“量身定做”骨缺损植入物,通过打印机1∶1成型骨缺损形状,解决了骨缺损外形匹配的难题[56]。此外,3D打印可实现仿生骨小梁结构,通过调节多孔结构参数使其弹性模量介于松质骨和皮质骨之间,避免应力遮挡,提高多孔钽植入体的初期稳定性,实现提高骨缺损修复植入体长期稳定性的目的[57-58]。"
| [1] CHRISTIAN AB, GRIGORIAN A, NAHMIAS J, et al. Comparison of surgical fixation and non-operative management in patients with traumatic sternum fracture. Eur J Trauma Emerg Surg. 2022;48(1): 219-224. [2] KLEI DS, ONER FC, LEENEN LPH, et al. Current treatment and outcomes of traumatic sternovertebral fractures: a systematic review. Eur J Trauma Emerg Surg. 2021;47(4):991-1001. [3] AMY X, CUO Y, CHENG LJ, et al. Biomedical applications of the powder-based 3D printed titanium alloys: A review. J Mater Sci Technol. 2022; 1125(4):252-264. [4] CHEN A, SU J, LI Y, et al. 3D/4D printed bio-piezoelectric smart scaffolds for next-generation bone tissue engineering. Int J Extr Manufacturing. 2023;5(3):242-268. [5] MOHAMMED AE, AHMED E, HIEDER AS, et al. Outcome of early surgical decompression in traumatic incomplete spinal cord injury. OJMN. 2020;6(10):353-363 [6] SAWADOGO M, TINTO S, DIALLO M, et al. Mortality of traumatic injuries in traumatological emergencies of the yalgado ouedraogo university hospital center in ouagadougou (Burkina Faso). Open J Orthop. 2022;9(12):33-39. [7] ABDELRAHMAN H, EL-MENYAR A, KEIL H, et al. Patterns, management, and outcomes of traumatic pelvic fracture: insights from a multicenter study. J Orthop Surg Res. 2020;15(1):249-252. [8] YURI BM, ANTONIO VNP, ANTONIO VNPF, et al. Retrospective epidemiological analysis of colles’ fracture in patients admitted in fernandes tavora hospital. Acta Biomater. 2023;1(13):16-23. [9] HENDAM H, TAHA A, YOUSSEF M, et al. Rod and screw fixation for cranio-cervical instability. Open J Modern Neurosurg. 2022;3(10):19-26. [10] 吴非,王子凡,王先辉,等.锁定加压钢板内固定治疗创伤性四肢骨折患者的疗效观察[J].贵州医药,2022,46(6):943-945. [11] CHRISTIAN BLOUGH. Stuart Harvey Kuschner.Distal radius fracture: what does the patient want? Open J Orthop. 2022;5(12):288-296. [12] ZHANG Z, YANG YQ, ZHANG HB, et al.3D Bio-printed bone scaffolds incorporated with natural antibacterial compounds. J Mater Sci Chem Eng. 2022;8(10):63-69. [13] SUN CH, SHANG GQ. Application and development of 3D printing in medical field. Modern Mechanical Engineering. 2020;11(10):25-33. [14] SHANG GQ, SUN CH. Effect of 3D printing technology on 3C product manufacturing. World J Eng Technol. 2020;17(8):712-719. [15] ANTNIO CST, MARIA IBT. Morphological, biological and physicochemical evaluation of abs-based systems containing graphene obtained by 3D printing via solution. Mater Sci Appl. 2022; 25(13):401-416. [16] KHANH Q, NGUYEN, PASCAL Y, et al.Recycled, bio-based, and blended composite materials for 3D printing filament: pros and cons—A review. Mater Sci Appl. 2023;20(14):148-185. [17] 张向南,邓伟,张松强,等.显微灌注结合3D打印制作股骨头内动脉铸型标本[J].中国临床解剖学杂志,2022,40(1):103-106,108. [18] GABALSKI MA, SMITH KR, HIX J, et al. Comparisons of 3D printed materials for biomedical imaging applications. Sci Technol Adv Mater. 2023;24(1):2273-2286. [19] ZHENG Y, DENG F, WANG B, et al. Melt extrusion deposition (MED™) 3D printing technology - a paradigm shift in design and development of modified release drug products. Int J Pharm. 2021;1(60):120-135. [20] AHMED H, HUSSAIN G, GOHAR S, et al. Impact toughness of hybrid carbon fiber-PLA/ABS laminar composite produced through fused filament fabrication. Polymers (Basel). 2021;13(18):3057-3061. [21] KHORSANDI D, FAHIMIPOUR A, ABASIAN P, et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021;1(122):26-49. [22] AL-DULIMI Z, WALLIS M, TAN DK, et al. 3D printing technology as innovative solutions for biomedical applications. Drug Discov Today. 2021;26(2):360-383. [23] VASILIADIS AV, KOUKOULIAS N, KATAKALOS K. From three-dimensional (3D)- to 6D-printing technology in orthopedics: science fiction or scientific reality? J Funct Biomater. 2022;13(3):101-102. [24] CHAROO NA, BARAKH ALI SF, MOHAMED EM, et al. Selective laser sintering 3D printing - an overview of the technology and pharmaceutical applications. Drug Dev Ind Pharm. 2020;46(6):869-877. [25] KESSLER A, HICKEL R, REYMUS M. 3D Printing in dentistry-state of the art. Oper Dent. 2020;45(1):30-40. [26] TABRIZ AG, GONOT-MUNCK Q, BAUDOUX A, et al. 3D Printing of personalised carvedilol tablets using selective laser sintering. Pharmaceutics. 2023;15(9):2230-2231. [27] CHEN N, LUO F, YANG G, et al. Production of Functional Materials Derived from Regenerated Silk Fibroin by Utilizing 3D Printing and Biomimetic Enzyme-induced Mineralization. Chin J Poly Sci. 2024; 42(3):299-310. [28] GUO A, ZHANG S, YANG R, et al. Enhancing the mechanical strength of 3D printed GelMA for soft tissue engineering applications. Mater Today Biol. 2023;30(24):1009-1010. [29] MENDONÇA CJA, GUIMARÃES RMDR, PONTIM CE, et al. An overview of 3D anatomical model printing in orthopedic trauma surgery. J Multidiscip Healthc. 2023;16:875-887. [30] ZHANG D, ZHANG X. Rehabilitation brace based on the internet of things 3d printing technology in the treatment and repair of joint trauma. J Healthc Eng. 2021;25(20):6663-6665. [31] MU Y, CHU Y, PAN L, et al. 3D printing critical materials for rechargeable batteries: from materials, design and optimization strategies to applications. Int J Extreme Manuf. 2023;5(4):219-250. [32] LYU Z, WANG J, CHEN Y. 4D printing: interdisciplinary integration of smart materials, structural design,and new functionality. Int J Extreme Manuf. 2023;5(3):348-367. [33] GAO Z, YIN J, LIU P, et al.Simultaneous multi-material embedded printing for 3D heterogeneous structures. Int J Extreme Manuf. 2023; 5(3):491-504. [34] 陈秋洪,程茂扬,曾华东,等.3D打印技术辅助切开复位空心钉内固定治疗复杂距骨骨折的疗效分析[J].中国骨与关节损伤杂志, 2021,36(10):1098-1100. [35] ZHOU H, YANG H, YAO S, et al. Synthesis of 3D printing materials and their electrochemical applications. Chin Chem Lett. 2022;33(8):3681-3694. [36] 高倚天,刘冰川,周方,等.3D打印假体在上肢围关节骨缺损治疗中的研究进展[J].生物骨科材料与临床研究,2024,21(2):65-70,76. [37] ZHANG H, SUN W. Mechanical properties and failure behavior of 3D printed thermoplastic composites using continuous basalt fiber under high-volume fraction. Defence Technol. 2023;27(9):237-250. [38] 郑轶,郑兴国,张嘉锴,等.基于3D金属打印技术锁骨近端解剖钢板的数字化研究[J].中国骨伤,2024,37(3):278-280. [39] LI X, SU H, DONG D, et al. Enhanced comprehensive properties of stereolithography 3D printed alumina ceramic cores with high porosities by a powder gradation design. J Mater Sci Technol. 2022; 131(36):264-275. [40] 魏东轩,周祥龙,熊蠡茗.3D打印截骨导板辅助胫骨骨折畸形愈合截骨矫形一例[J].临床外科杂志,2024,32(3):335-336. [41] 王芳芳,石家晓,苏冬冬,等.3D打印人工椎体辅助SRS-SchwabⅣ级截骨术治疗创伤后胸腰段后凸畸形的临床应用[J].中国煤炭工业医学杂志,2024,27(1):78-83. [42] CHOO YJ, BOUDIER-REVERET M, CHANG MC. 3D printing technology applied to orthosis manufacturing: narrative review. Ann Palliat Med. 2020;9(6):4262-4270. [43] MENG M, WANG J, SUN T, et al. Clinical applications and prospects of 3D printing guide templates in orthopaedics. J Orthop Translat. 2022;13(34):22-41. [44] XIN X, LIU X, ZHU Y, et al. 3D-printed guide plate system-assisted thoracolumbar kyphosis osteotomy: a technical case series. World Neurosurg. 2023;17(3):28-33. [45] ZHOU L, WANG W, LI Z, et al. Clinical application of 3D-Slicer + 3D printing guide combined with transcranial neuroendoscopic in minimally invasive neurosurgery. Sci Rep. 2022;12(1):2042-2043. [46] WU H, YANG S, LIU J, et al. 3D printing guide plate for accurate hemicortical bone tumor resection in metaphysis of distal femoral: a technical note. J Orthop Surg Res. 2021;16(1):343-345. [47] KEYU G, SHUAISHUAI L, RAJ A, et al. A 3D printing personalized percutaneous puncture guide access plate for percutaneous nephrolithotomy: a pilot study. BMC Urol. 2021;21(1):184-186. [48] LI L, LUO Z, GUAN H, et al. Design and localization algorithm of flap guide plate for jaw defect based on digital 3D printing. Prev Med. 2023;17(3):1075-1078. [49] 刘爱国,陈朝辉,李东辉,等.下颈椎骨折并脱位手术中3D打印导航模板的有效性与安全性评价[J].深圳中西医结合杂志,2022, 32(6):6-9. [50] 谢斌,苏晨晨.Gamma3钉内固定结合3D打印治疗AOA3型老年股骨粗隆间骨折的疗效分析[J].贵州医药,2023,47(10):1577-1578. [51] HA SH, JUNG S, CHOI JY. Reduction malarplasty using customized surgical stent based on 3D virtual surgery, CAD/CAM, and 3D printing technology: case series. J Craniofac Surg. 2022;33(5): 1578-1582. [52] HAN X, SAIDING Q, CAI X, et al. Intelligent vascularized 3D/4D/5D/6D-printed tissue scaffolds. Nanomicro Lett. 2023;15(1):239-252. [53] ZHANG C, SONG C, WANG D, et al. Digitally driven surgical guide planning. J Clin Pediatr Dent. 2024;48(1):128-137. [54] KANG S, ZHAO C, FAN Y. Puncture and drainage surgery for intracerebral hemorrhage guided by 3d printing puncture guide plate. J Craniofac Surg. 2024;35(4):1264-1267. [55] TANG X, LAI Q, XUE R, et al. Hard tissue preservation and recovery in minimally invasive alveolar surgery using three-dimensional printing guide plate. J Craniofac Surg. 2022;33(5): e476-e481. [56] HA SH, OH JS, JEONG CG, et al. The efficacy of 3D virtual surgery, CAD/CAM, and 3D printing technology for maxillomandibular advancement in obstructive sleep apnea patients. J Craniofac Surg. 2023;34(3):300-304. [57] ROY T, STEINBACHER DM. Virtual planning and 3D printing in contemporary orthognathic surgery. Semin Plast Surg. 2022;36(3): 169-182. [58] 张阳.3D打印明胶/海藻酸钠/58S生物玻璃骨缺损修复支架的生物安全性评价[J].中国组织工程研究,2022,26(4):521-527. [59] 冯刚,吴怡梵.3D打印结合镜像模型在创伤骨科教学培训中的应用研究[J].全科医学临床与教育,2024,22(3):250-252. [60] 高博,吴碧,阎敏,等.3D打印导向器与导航下引导骶髂螺钉置入的对比研究[J].实用骨科杂志,2024,30(3):222-225,237. |
| [1] | Yu Shuai, Liu Jiawei, Zhu Bin, Pan Tan, Li Xinglong, Sun Guangfeng, Yu Haiyang, Ding Ya, Wang Hongliang. Hot issues and application prospects of small molecule drugs in treatment of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1913-1922. |
| [2] | Yu Jingbang, Wu Yayun. Regulatory effect of non-coding RNA in pulmonary fibrosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1659-1666. |
| [3] | Wang Qiuyue, Jin Pan, Pu Rui . Exercise intervention and the role of pyroptosis in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1667-1675. |
| [4] | Yuan Weibo, Liu Chan, Yu Limei. Potential application of liver organoids in liver disease models and transplantation therapy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1684-1692. |
| [5] | Peng Hongcheng, Peng Guoxuan, Lei Anyi, Lin Yuan, Sun Hong, Ning Xu, Shang Xianwen, Deng Jin, Huang Mingzhi . Role and mechanism of platelet-derived growth factor BB in repair of growth plate injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1497-1503. |
| [6] | Liu Haoyang, Xie Qiang, Shen Mengran, Ren Yansong, Ma Jinhui, Wang Bailiang, Yue Debo, Wang Weiguo . Application, research hotspots, and shortcomings of degradable zinc-based alloys in bone defect repair and reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 839-845. |
| [7] | Guo Zhao, Zhuang Haoyan, Shi Xuewen. Role of exosomes derived from mesenchymal stem cells in treatment of colorectal cancer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7872-7879. |
| [8] | Huang Haina, Yu Yanrong, Bi Jian, Huang Miao, Peng Weijie. Epigenetic characteristics of hepatogenic differentiation of mesenchymal stem cells in three-dimensional culture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7848-7855. |
| [9] | Liu Lu, Zhong Chang, Yu Xin, Ren Chenyuan, Gong Yangyang, Zhou Ping, Wang Yingbin. Academic progress and clinical application of in vitro synthetic microenvironment to promote maturation of human pluripotent stem cell-derived cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7856-7862. |
| [10] | Su Yongkun, Sun Hong, Liu Miao, Yang Hua, Li Qingsong. Development of novel antioxidants and antioxidant combination carried by nano-hydrogel systems in treatment of intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7376-7384. |
| [11] | Yi Xiaoding, Zhang Di, Guo Hong, Qing Liang, Zhao Tianyu. Decellularized tendon scaffold: a biomedical material for tendon injury repair [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7385-7392. |
| [12] | Li Zhongzheng, Chen Zhenghao, Tang Ziyou, Lou Kaiyang, Zhang Rui, Liu Qi, Zhao Na, Yang Kun. Effects of scaffold materials combined with biological factors on biological characteristics of dental follicle cell proliferation and osteogenic differentiation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7405-7414. |
| [13] | Zhang Pulian, Liu Baoru, Yang Min . Mesenchymal stem cells for treatment of aplastic anemia: inhibiting or activating relevant targets in its pathological evolution [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6800-6810. |
| [14] | Zhao Xiaoxuan, Liu Shuaiyi, Xing Zheng, Li Qingwen, Chu Xiaolei, Li Qi. Research hotspots and trends in application of tissue engineering in peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6591-6600. |
| [15] | Yang Cheng, Li Weimin, Ran Dongcheng, Xu Jiamu, Wu Wangxiang, Xu Jiafu, Chen Jingjing, Jiang Guangfu, Wang Chunqing. Ferroptosis and osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 554-562. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||