Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (20): 4223-4229.doi: 10.12307/2025.674
Previous Articles Next Articles
Effects of visual interference on biomechanical characteristics of lower limbs in athletes after anterior cruciate ligament reconstruction
Zhang Sizhuo1, 2, Liu Xiaoqian1, Wang Guanglan2
- 1Wuhan Business University, Wuhan 430079, Hubei Province, China; 2School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China
-
Received:2024-07-17Accepted:2024-08-31Online:2025-07-18Published:2024-12-20 -
Contact:Wang Guanglan, MS, Professor, Master’s supervisor, School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China -
About author:Zhang Sizhuo, MS, Lecturer, Wuhan Business University, Wuhan 430079, Hubei Province, China -
Supported by:Wuhan Business School School-Level Project, No. [2023]1+2023KY037 (to ZSZ); Hubei Provincial Department of Education Science and Technology Research Program Guidance Project, No. B2022294 (to LXQ)
CLC Number:
Cite this article
Zhang Sizhuo, Liu Xiaoqian, Wang Guanglan. Effects of visual interference on biomechanical characteristics of lower limbs in athletes after anterior cruciate ligament reconstruction[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4223-4229.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
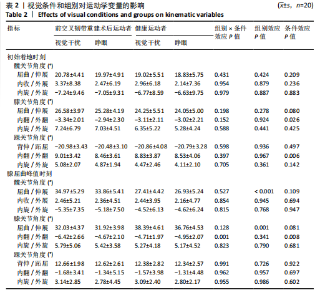
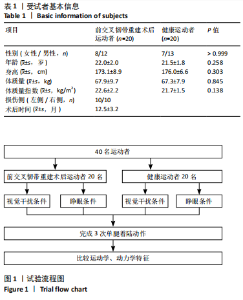
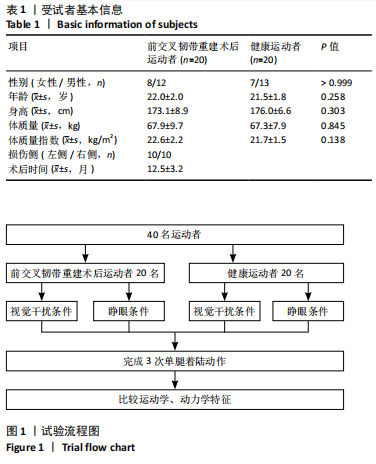
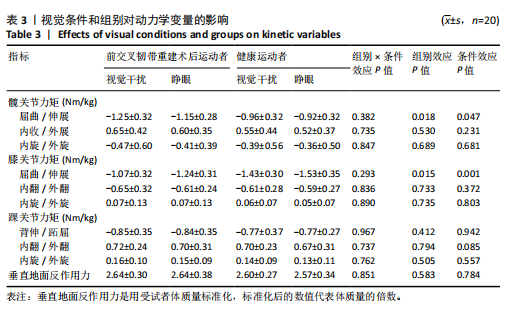
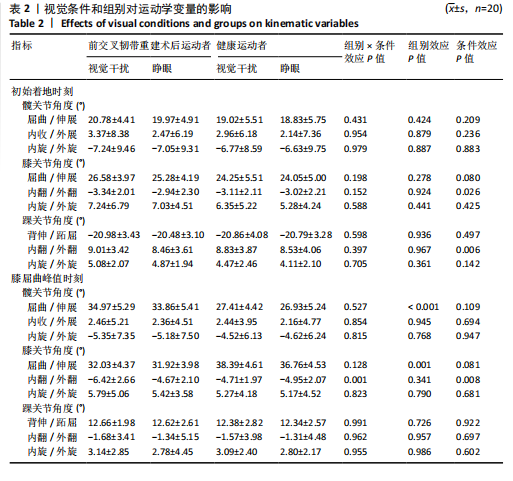
视觉干扰条件下的膝关节外翻角度(P=0.026)和踝关节内翻角度(P=0.006)显著升高,见表2。 膝关节屈曲角度峰值时刻,膝关节外翻角度存在显著的交互效应(P=0.001)。事后分析显示,与睁眼条件相比,视觉干扰条件下前交叉韧带重建术后运动者膝关节外翻角度显著升高(P < 0.001)。健康运动者膝关节外翻角度在两种视觉条件下无显著差异(P=0.527)。此外,视觉干扰条件下,前交叉韧带重建术后运动者膝关节外翻角度显著高于健康运动者(P=0.048),见表2。 膝关节屈曲峰值角度时刻,髋关节屈曲角度和膝关节屈曲角度不存在交互效应(P=0.527,P=0.128),但具有显著的组别主效应(P < 0.001,P=0.001)。与健康运动者相比,前交叉韧带重建术后运动者髋关节屈曲角度更高(P < 0.001),膝关节屈曲角度更低(P=0.001),见表2。 2.5 动力学变量 膝关节屈曲峰值角度时刻,髋关节伸直力矩和膝关节伸直力矩不存在交互效应(P=0.382,P=0.293),但具有显著的条件主效应和组别主效应(P < 0.05)。与睁眼条件相比,视觉干扰条件下的髋关节伸直力矩显著升高(P=0.047),膝关节伸直力矩显著降低(P=0.001)。与健康运动者相比,前交叉韧带重建术后运动者髋关节伸直力矩更高(P=0.018),膝关节伸直力矩更低(P=0.015),见表3。 2.6 不良事件 测试期间40名受试者未发生运动损伤等不良事件。"
| [1] MONTALVO AM, SCHNEIDER DK, WEBSTER KE, et al. Anterior Cruciate Ligament Injury Risk in Sport: A Systematic Review and Meta-Analysis of Injury Incidence by Sex and Sport Classification. J Athl Train. 2019; 54(5):472-482. [2] ZHANG S, WANG L, LIU X, et al. Effects of Kinesio taping on lower limb biomechanical characteristics during the cutting maneuver in athletes after anterior cruciate ligament reconstruction. PLoS One. 2024;19(3):e0299216. [3] PASCHOS NK, HOWELL SM. Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev. 2016;1(11):398-408. [4] ZHANG L, JIANG K, CHAI H, et al. A Comparative Animal Study of Tendon Grafts Healing After Remnant-Preserving Versus Conventional Anterior Cruciate Ligament Reconstruction. Med Sci Monit. 2016;22:3426-3437. [5] LEE BI, KIM CH, JANG BW, et al. Preservation of the Tibial Remnant in Anterior Cruciate Ligament Reconstruction May Improve Postoperative Proprioceptive Function. Orthopedics. 2020;43(4):e231-e236. [6] RELPH N, HERRINGTON L, TYSON S. The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy. 2014;100(3):187-195. [7] AGEBERG E, FRIDéN T. Normalized motor function but impaired sensory function after unilateral non-reconstructed ACL injury: patients compared with uninjured controls. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):449-456. [8] JOHNSTON PT, MCCLELLAND JA, WEBSTER KE. Lower Limb Biomechanics During Single-Leg Landings Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med. 2018;48(9):2103-2126. [9] LEPLEY AS, KUENZE CM. Hip and Knee Kinematics and Kinetics During Landing Tasks After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. J Athl Train. 2018;53(2):144-159. [10] CRONSTRöM A, AGEBERG E. Association between sensory function and medio-lateral knee position during functional tasks in patients with anterior cruciate ligament injury. BMC Musculoskelet Disord. 2014;15:430. [11] CINQUE ME, DORNAN GJ, CHAHLA J, et al. High Rates of Osteoarthritis Develop After Anterior Cruciate Ligament Surgery: An Analysis of 4108 Patients. Am J Sports Med. 2018;46(8):2011-2019. [12] DINGENEN B, JANSSENS L, LUYCKX T, et al. Postural stability during the transition from double-leg stance to single-leg stance in anterior cruciate ligament injured subjects. Clin Biomech (Bristol, Avon). 2015; 30(3):283-289. [13] TECCO S, SALINI V, CALVISI V, et al. Effects of anterior cruciate ligament (ACL) injury on postural control and muscle activity of head, neck and trunk muscles. J Oral Rehabil. 2006;33(8):576-587. [14] GROOMS D, APPELBAUM G, ONATE J. Neuroplasticity following anterior cruciate ligament injury: a framework for visual-motor training approaches in rehabilitation. J Orthop Sports Phys Ther. 2015;45(5): 381-393. [15] PETERKA RJ. Sensory integration for human balance control. Handb Clin Neurol. 2018;159:27-42. [16] DOSHER B, LU ZL. Visual Perceptual Learning and Models. Annu Rev Vis Sci. 2017;3:343-363. [17] XUE X, WANG Y, XU X, et al. Postural Control Deficits During Static Single-leg Stance in Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Sports Health. 2024;16(1):29-37. [18] WIKSTROM EA, SONG K, PIETROSIMONE BG, et al. Visual Utilization During Postural Control in Anterior Cruciate Ligament- Deficient and -Reconstructed Patients: Systematic Reviews and Meta-Analyses. Arch Phys Med Rehabil. 2017;98(10):2052-2065. [19] LOUW Q, GILLION N, VAN NIEKERK SM, et al. The effect of vision on knee biomechanics during functional activities - A systematic review. J Sci Med Sport. 2015;18(4):469-474. [20] WARD S, PEARCE AJ, PIETROSIMONE B, et al. Neuromuscular deficits after peripheral joint injury: a neurophysiological hypothesis. Muscle Nerve. 2015;51(3):327-332. [21] DHILLON MS, BALI K, PRABHAKAR S. Proprioception in anterior cruciate ligament deficient knees and its relevance in anterior cruciate ligament reconstruction. Indian J Orthop. 2011;45(4):294-300. [22] WOHL TR, CRISS CR, GROOMS DR. Visual Perturbation to Enhance Return to Sport Rehabilitation after Anterior Cruciate Ligament Injury: A Clinical Commentary. Int J Sports Phys Ther. 2021;16(2):552-564. [23] HOOTMAN JM, DICK R, AGEL J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319. [24] MCKAY GD, GOLDIE PA, PAYNE WR, et al. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103-108. [25] SCHMITT LC, PATERNO MV, FORD KR, et al. Strength Asymmetry and Landing Mechanics at Return to Sport after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc. 2015;47(7):1426-1434. [26] HAN S, LEE H, SON SJ, et al. The effects of visual feedback disruption on postural control with chronic ankle instability. J Sci Med Sport. 2022;25(1):53-57. [27] LEE H, HAN S, SON SJ, et al. Disrupted vision impairs force steadiness and accuracy in chronic ankle instability patients. J Orthop Res. 2023; 41(8):1729-1737. [28] LIU Q, WANG L, DAI F, et al. Effects of ankle Kinesio taping on knee and ankle joint biomechanics during unanticipated jumps in collegiate athletes. PLoS One. 2024;19(8):e0305480. [29] WANG L, CHEN P, DING Y, et al. Effects of Kinesio taping on lower limb biomechanical characteristics during unexpected jumping in patients with chronic ankle instability. Scand J Med Sci Sports. 2024; 34(1):e14566. [30] LEPLEY LK, WOJTYS EM, PALMIERI-SMITH RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve biomechanical limb symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2015;30(7):738-747. [31] LEE H, HAN S, HOPKINS JT. Visual Disruption Influences Neuromechanics during Landing Cutting in Individuals with Chronic Ankle Instability. J Athl Train. 2024;59(8):822-829. [32] CHEN P, WANG L, DONG S, et al. Abnormal Lower Limb Biomechanics During a Bilateral Vertical Jump Despite the Symmetry in Single-Leg Vertical Hop Height in Athletes After ACL Reconstruction. Orthop J Sports Med. 2024;12(2):23259671241230989. [33] HEWETT TE, MYER GD, FORD KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299-311. [34] SONG K, KANG TK, WIKSTROM EA, et al. Effects of reduced plantar cutaneous sensation on static postural control in individuals with and without chronic ankle instability. J Sci Med Sport. 2017;20(10):910-914. [35] MCKEON PO, HERTEL J. Plantar hypoesthesia alters time-to-boundary measures of postural control. Somatosens Mot Res. 2007;24(4):171-177. [36] McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. [37] GROOMS DR, CHAUDHARI A, PAGE SJ, et al. Visual-Motor Control of Drop Landing After Anterior Cruciate Ligament Reconstruction. J Athl Train. 2018;53(5):486-496. [38] XU Y, SONG B, MING A, et al. Chronic ankle instability modifies proximal lower extremity biomechanics during sports maneuvers that may increase the risk of ACL injury: A systematic review. Front Physiol. 2022;13:1036267. [39] EMAMVIRDI M, HOSSEINZADEH M, LETAFATKAR A, et al. Comparing kinematic asymmetry and lateral step-down test scores in healthy, chronic ankle instability, and patellofemoral pain syndrome female basketball players: a cross-sectional study. Sci Rep. 2023;13(1):12412. [40] WREN TAL, MUESKE NM, BROPHY CH, et al. Hop Distance Symmetry Does Not Indicate Normal Landing Biomechanics in Adolescent Athletes With Recent Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2018;48(8):622-629. [41] 陈鹏,左会武,王玲,等.前交叉韧带重建术后运动者单腿垂直跳跃高度对称性掩盖其异常下肢生物力学[J].中国运动医学杂志, 2023,42(12):939-947. [42] CHEN P, WANG L, DONG S, et al. Can Symmetry of Single-Leg Vertical Jump Height Represent Normal Lower Limb Biomechanics of Athletes After Anterior Cruciate Ligament Reconstruction? Sports Health. 2024; 16(4):596-605. [43] OIESTAD BE, HOLM I, AUNE AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201-2210. [44] SRITHARAN P, MUñOZ MA, PIVONKA P, et al. Biomechanical Markers of Forward Hop-Landing After ACL-Reconstruction: A Pattern Recognition Approach. Ann Biomed Eng. 2022;50(3):330-342. [45] KIM H, SON SJ, SEELEY MK, et al. Kinetic Compensations due to Chronic Ankle Instability during Landing and Jumping. Med Sci Sports Exerc. 2018;50(2):308-317. [46] SYMEONIDOU ER, FERRIS DP. Visual Occlusions Result in Phase Synchrony Within Multiple Brain Regions Involved in Sensory Processing and Balance Control. IEEE Trans Neural Syst Rehabil Eng. 2023;31:3772-3780. [47] KIM KM, KIM JS, GROOMS DR. Stroboscopic Vision to Induce Sensory Reweighting During Postural Control. J Sport Rehabil. 2017;26(5):1-11. [48] CLARK JF, ELLIS JK, BENCH J, et al. High-performance vision training improves batting statistics for University of Cincinnati baseball players. PLoS One. 2012;7(1):e29109. [49] MITROFF SR, FRIESEN P, BENNETT D, et al. Enhancing ice hockey skills through stroboscopic visual training: a pilot study. Athletic Training & Sports Health Care. 2013;5(6):261-264. [50] HüLSDüNKER T, GUNASEKARA N, MIERAU A. Short- and Long-Term Stroboscopic Training Effects on Visuomotor Performance in Elite Youth Sports. Part 1: Reaction and Behavior. Med Sci Sports Exerc. 2021;53(5):960-972. [51] HüLSDüNKER T, GUNASEKARA N, MIERAU A. Short- and Long-Term Stroboscopic Training Effects on Visuomotor Performance in Elite Youth Sports. Part 2: Brain-Behavior Mechanisms. Med Sci Sports Exerc. 2021; 53(5):973-985. |
| [1] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [2] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [3] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [4] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [5] | Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904. |
| [6] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [7] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [8] | Zhuang Yan, Wang Xinyu, Cao Yilin, Ding Yuanxin, Wang Jiaqi, Yu Miao, Luan Chunyang, Ding Yuansheng. Three-dimensional finite element analysis of personalized orthodontic devices for 3D printed maxillary single-rooted rotated tooth [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6409-6415. |
| [9] | He Kai, Xing Wenhua, Liu Shengxiang, Bai Xianming, Zhou Chen, Gao Xu, Qiao Yu, He Qiang, Gao Zhiyu, Guo Zhen, Bao Aruhan, Li Chade. Constructing a model of degenerative scoliosis using finite element method: biomechanical analysis in etiology and treatment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 572-578. |
| [10] | Gao Xilin, Wu Si Zhang Chao Zhu Liguo, Fu Bifeng, Wang Ping. Mechanotransduction proteins in intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 579-589. |
| [11] | Wang X, Wang Hm, Chen Sh, Feng Tx, Bu Hm, Zhu Lg, Chen Dd, Wei X. Stress and morphological characteristics of intervertebral foramen of cervical rotation-traction manipulation for treating cervical spondylotic radiculopathy: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 441-447. |
| [12] | Zhao Yuxin, Liang Liang, Jin Feng, Xu Yangyang, Kang Zhijie, Fang Yuan, He Yujie, Wang Xing, Wang Haiyan, Li Xiaohe. Establishment and stress analysis of a finite element model for adolescent cervical disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 448-454. |
| [13] | Li Zhenggang, Shang Xuehong, Wu Zhang, Li Hong, Sun Chaojun, Chen Huadong, Sun Zhe, Yang Yi. Finite element analysis of three internal fixation modalities for treatment of Pauwels type III femoral neck fractures under different loading conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 455-463. |
| [14] | Liu Mengfei, Chen Gang, Shi Yihan, Zeng Lin, Jiang Kan, Yilihamujiang•Wusiman. Finite element analysis of optimization of femoral prosthesis implantation position in unicompartmental knee arthroplasty in osteoporotic patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 464-470. |
| [15] | Gou Yanyun, Hou Meijin, Jiang Zheng, Chen Shaoqing, Chen Xiang, Gao Yuzhan, Wang Xiangbin. Biomechanical characteristics of walking in patients with idiopathic scoliosis: cross-sectional analysis of three-dimensional motion capture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 471-477. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||