[1] SAVIN IA, ZENKOVA MA, SEN’KOVA AV. Pulmonary Fibrosis as a Result of Acute Lung Inflammation: Molecular Mechanisms, Relevant In Vivo Models, Prognostic and Therapeutic Approaches. Int J Mol Sci. 2022;23(23):14959.
[2] WU Q, ZHANG KJ, JIANG SM, et al. p53: A Key Protein That Regulates Pulmonary Fibrosis. Oxid Med Cell Longev. 2020;2020:6635794.
[3] 中华人民共和国国家卫生健康委员会.2020年我国卫生健康事业发展统计公报[J].中国实用乡村医生杂志,2021,28(9):1-10.
[4] WANG J, BAO A, GU J, et al. A retrospective analysis of 12,400 SARS-CoV-2 RNA tests in patients with COVID-19 in Wuhan. Medicine (Baltimore). 2021;100(20): e25916.
[5] WU M, WANG Z, SHI X, et al. TGFβ1-RCN3-TGFBR1 loop facilitates pulmonary fibrosis by orchestrating fibroblast activation. Respir Res. 2023;24(1):222.
[6] 冀会鸽,李亚,余学庆.中医药干预肺纤维化相关信号通路研究进展[J].中国中医药现代远程教育,2019,17(4):124-126.
[7] 石祥广.肺纤维化的”前世今生”[J].张江科技评论,2021(4):12-15.
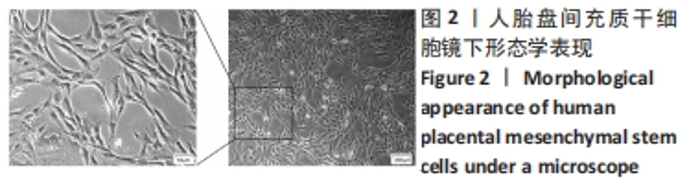
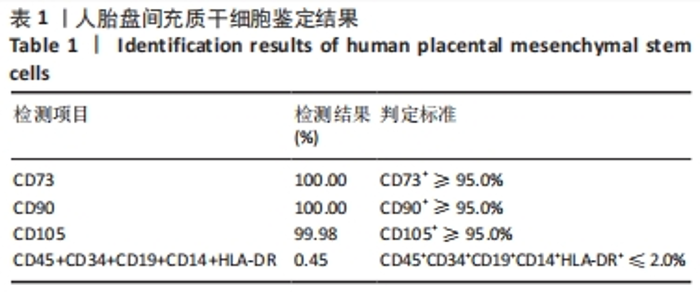
[8] HAN ZB, WANG YW, WANG T, et al. Isolation and biological characteristics of mesenchymal stem cells derived from human placenta decidua basalis. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2013;21(3):754-759.
[9] MANSOURI N, WILLIS GR, FERNANDEZ-GONZALEZ A, et al. Mesenchymal stromal cell exosomes prevent and revert experimental pulmonary fibrosis through modulation of monocyte phenotypes. JCI Insight. 2019;4(21):e128060.
[10] CRUZ FF, ROCCO PRM. The potential of mesenchymal stem cell therapy for chronic lung disease. Expert Rev Respir Med. 2020;14(1):31-39.
[11] PARIS JL, DE LA TORRE P, CABAÑAS MV, et al. Suicide-gene transfection of tumor-tropic placental stem cells employing ultrasound-responsive nanoparticles. Acta Biomater. 2019;83:372-378.
[12] SHAFIEE A, PATEL J, LEE JS, et al. Mesenchymal stem/stromal cells enhance engraftment, vasculogenic and pro-angiogenic activities of endothelial colony forming cells in immunocompetent hosts. Sci Rep. 2017;7(1):13558.
[13] WHITLOCK AE, MOSKOWITZOVA K, KYCIA I, et al. Morphometric, Developmental, and Anti-Inflammatory Effects of Transamniotic Stem Cell Therapy (TRASCET) on the Fetal Heart and Lungs in a Model of Intrauterine Growth Restriction. Stem Cells Dev. 2023;32(15-16):484-490.
[14] ZWOLANEK D, SATUÉ M, PROELL V, et al. Tracking mesenchymal stem cell contributions to regeneration in an immunocompetent cartilage regeneration model. JCI Insight. 2017;2(20):e87322.
[15] WU S, YIN L, HAN K, et al. NAT10 accelerates pulmonary fibrosis through N4-acetylated TGFB1-initiated epithelial-to-mesenchymal transition upon ambient fine particulate matter exposure. Environ Pollut. 2023;322:121149.
[16] WIJSENBEEK M, COTTIN V. Spectrum of Fibrotic Lung Diseases. N Engl J Med. 2020;383(10):958-968.
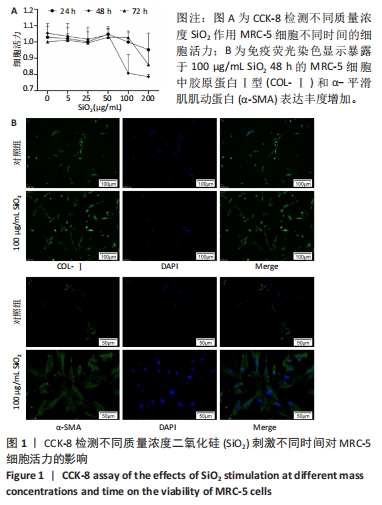
[17] MA J, CAI Q, YANG D, et al. A Positive Feed Forward Loop between Wnt/β-Catenin and NOX4 Promotes Silicon Dioxide-Induced Epithelial-Mesenchymal Transition of Lung Epithelial Cells. Oxid Med Cell Longev. 2020;2020:3404168.
[18] 韩闪,刘晓秋.嗜酸性粒细胞与特发性肺纤维化关系的研究进展[J].中华实用诊断与治疗杂志,2021,35(11):1182-1184.
[19] 沈怡,李雅倩,胡晓燕,等.生物标志物在特发性肺纤维化中的研究进展[J].临床肺科杂志,2021,26(4):589-593.
[20] CICCHINI C, AMICONE L, ALONZI T, et al. Molecular mechanisms controlling the phenotype and the EMT/MET dynamics of hepatocyte. Liver Int. 2015;35(2): 302-310.
[21] ZHANG L, WANG Y, WU G, et al. Macrophages: friend or foe in idiopathic pulmonary fibrosis? Respir Res. 2018;19(1):170.
[22] MA TT, MENG XM. TGF-β/Smad and Renal Fibrosis. Adv Exp Med Biol. 2019;1165: 347-364.
[23] XU F, LIU C, ZHOU D, et al. TGF-β/SMAD Pathway and Its Regulation in Hepatic Fibrosis. J Histochem Cytochem. 2016;64(3):157-167.
[24] ZHAO R, LI N, XU J, et al. Quantitative single-molecule study of TGF-β/Smad signaling. Acta Biochim Biophys Sin (Shanghai). 2018;50(1):51-59.
[25] JI WJ, ZHOU X, ZENG S, et al. Attenuation of silica-induced pulmonary fibroblasts proliferation by taurine and niacin in vitro. Exp Lung Res. 2009;35(3):198-209.
[26] SAMAH M, EL-AIDY AEL-R, TAWFIK MK, et al. Evaluation of the antifibrotic effect of fenofibrate and rosiglitazone on bleomycin-induced pulmonary fibrosis in rats. Eur J Pharmacol. 2012;689(1-3):186-193.
[27] ZHANG T, LIANG L, LIU X, et al. TGFβ1-Smad3-Jagged1-Notch1-Slug signaling pathway takes part in tumorigenesis and progress of tongue squamous cell carcinoma. J Oral Pathol Med. 2016;45(7):486-493.
[28] 丁志丹,王跃斌,李丰科,等.双肺移植同期冠状动脉旁路移植术治疗特发性肺纤维化合并冠心病1例临床分析[J]. 中华实用诊断与治疗杂志,2022, 36(11):1081-1085.
[29] XIAO K, HE W, GUAN W, et al. Mesenchymal stem cells reverse EMT process through blocking the activation of NF-κB and Hedgehog pathways in LPS-induced acute lung injury. Cell Death Dis. 2020;11(10):863.
[30] YANG S, LIU P, JIANG Y, et al. Therapeutic Applications of Mesenchymal Stem Cells in Idiopathic Pulmonary Fibrosis. Front Cell Dev Biol. 2021;9:639657.
[31] ZHAO Y, YAN Z, LIU Y, et al. Effectivity of mesenchymal stem cells for bleomycin-induced pulmonary fibrosis: a systematic review and implication for clinical application. Stem Cell Res Ther. 2021;12(1):470.
[32] LI F, HAN F, LI H, et al. Human placental mesenchymal stem cells of fetal origins-alleviated inflammation and fibrosis by attenuating MyD88 signaling in bleomycin-induced pulmonary fibrosis mice. Mol Immunol. 2017;90:11-21.
[33] TAO J, LI Q, MA X, et al. Human placental mesenchymal stem cells of fetal origin relieves mouse pulmonary fibrosis via downregulating MyD88 and TGF-β signaling pathway. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2016;32(10):1347-1351.
|