Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (17): 2625-2630.doi: 10.12307/2024.475
Calcium phosphate combined with recombinant human bone morphogenetic protein-2 in repair and reconstruction of tibial infectious bone defects
Jia Xufeng1, Long Miao2, Huang Guangping1, Zhong Qing3, Zhang Zhaoyao1, Qi Yuxin1, Tian Peng1, Li Ping1, Chen Yuchi4
- 1Department of Orthopedics, 2Department of Ultrasound, 3Department of Anesthesiology, 4Department of Radiology, Jianyang Hospital, Southwest Medical University • The People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China
-
Received:2023-07-12Accepted:2023-08-30Online:2024-06-18Published:2023-12-14 -
Contact:Huang Guangping, MD, Chief physician, Master’s supervisor, Department of Orthopedics, Jianyang Hospital, Southwest Medical University • The People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China Zhong Qing, Master, Chief physician, Master’s supervisor, Department of Anesthesiology, Jianyang Hospital, Southwest Medical University • The People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China -
About author:Jia Xufeng, Master, Master’s supervisor, Associate chief physician, Department of Orthopedics, Jianyang Hospital, Southwest Medical University • The People’s Hospital of Jianyang City, Jianyang 641400, Sichuan Province, China -
Supported by:Sichuan Medical Research Project, No. S20037 (to ZQ); Scientific Research Project of Sichuan Provincial Health and Planning Commission, No. 17PJ212 (to HGP); Scientific Research Project of Chengdu Jianyang Health Commission, No. 2020085 (to ZZY)
CLC Number:
Cite this article
Jia Xufeng, Long Miao, Huang Guangping, Zhong Qing, Zhang Zhaoyao, Qi Yuxin, Tian Peng, Li Ping, Chen Yuchi. Calcium phosphate combined with recombinant human bone morphogenetic protein-2 in repair and reconstruction of tibial infectious bone defects[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(17): 2625-2630.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
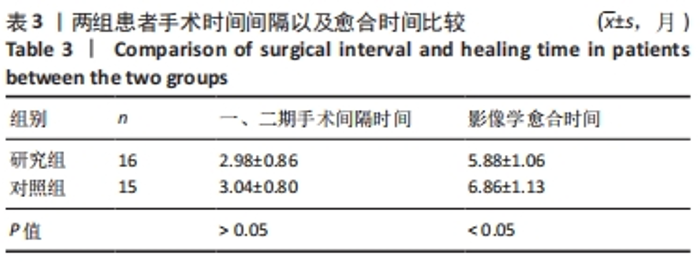
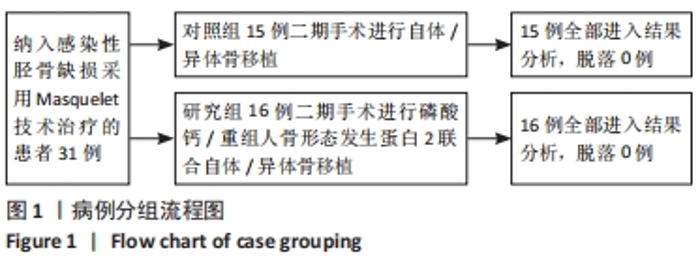
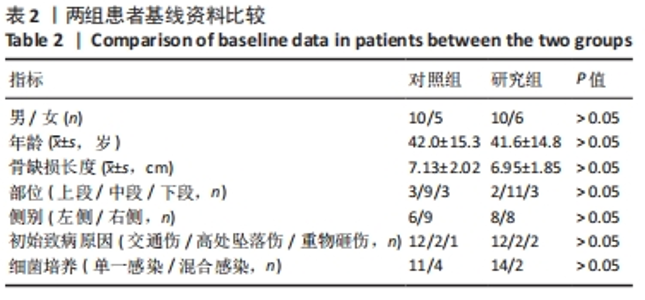
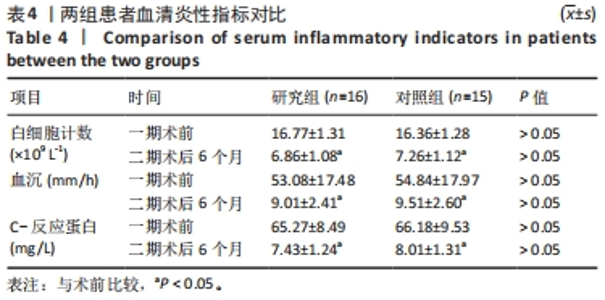
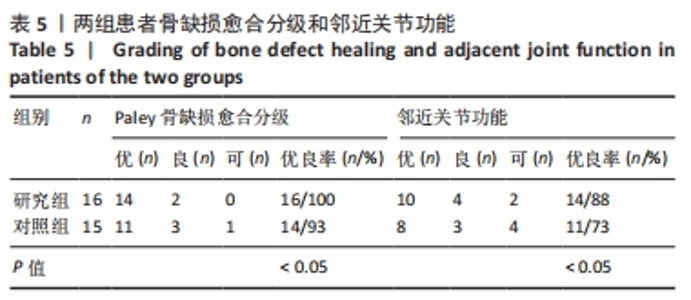
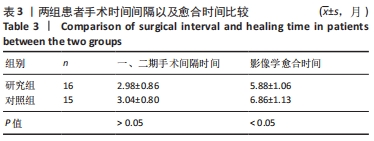
2.4 两组患者一般指标比较 所有患者经使用旷置假体后感染控制,行二期植骨手术后切口均有效愈合。两组患者一、二期手术间隔时间分别为(2.98±0.86),(3.04±0.80)个月,组间比较差异无显著性意义(P > 0.05),两组患者双侧肢体长度恢复对比良好。两组患者随访时间为6-36个月,研究组平均随访(16.3±8.4)个月,对照组平均随访(16.1±8.5)个月,组间比较差异无显著性意义(P > 0.05)。研究组有14例(88%)患者骨缺损获得修复,影像学愈合时间为(5.88±1.06)个月;对照组有11例(73%)患者骨缺损获得修复,影像学愈合时间为(6.86±1.13)个月,组间比较差异有显著性意义(P < 0.05),见表3。"
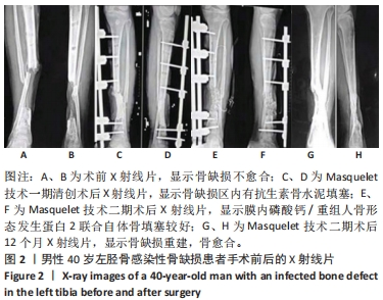
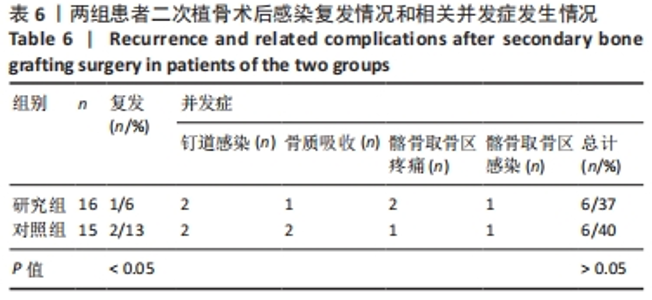
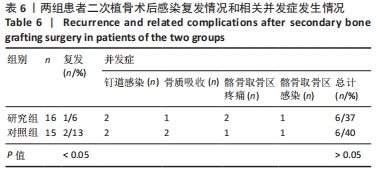
二次植骨术后感染复发情况:研究组有1例感染复发,为术后3个月,复发率为6%,对其进行重新清创、植骨、固定后感染控制,功能恢复。对照组有2例感染复发,分别为术后1,8个月,复发率为13%,其中1例进行重新清创、植骨、固定后感染控制,功能恢复,另1例因深部感染未能控制,后期行截肢手术。两组感染复发率比较差异有显著性意义(P < 0.05)。 其他相关并发症:研究组和对照组各有2例发生钉道感染,仔细清理钉道后对症治疗有3例感染治愈,对照组有1例感染未能控制,后期行截肢手术。研究组和对照组分别有1,2例在植骨后出现骨质吸收、延迟愈合,给予再次植骨后骨愈合。研究组和对照组分别有2,1例发生髂骨取骨区疼痛,给予止痛处理后缓解。研究组和对照组各有1例发生髂骨取骨区感染,经重新清创后治愈。研究组使用磷酸钙/重组人骨形态发生蛋白2后未发现异位骨化、骨溶解、过度炎症反应等并发症。两组并发症发生率比较差异无显著性意义(P > 0.05)。 2.9 典型病例分析 40岁男性患者,车祸致左胫骨骨折,伤后在当地医院行切开复位、钢板固定术。术后15 d伤口感染,行常规换药处理并静脉滴注抗生素2周,伤口渗液持续存在,术后2个月来简阳市人民医院就诊,行清创术,彻底清除所有的血肿、坏死组织、死骨及增生的肉芽组织,清创后植入抗生素骨水泥;2个月取出抗生素骨水泥占位器,骨缺损中央填充植骨颗粒,然后将磷酸钙/重组人骨形态发生蛋白2填充骨缺损外周。植骨后3个月骨缺损初步愈合,12个月骨折愈合良好。该患者影像学资料,见图2。"

| [1] WANG J, YIN Q, GU S, et al. Induced membrane technique in the treatment of infectious bone defect: A clinical analysis. Orthop Traumatol Surg Res. 2019; 105(3):535-539. [2] AKTUGLU K, EROL K, VAHABI A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20(1):22. [3] Lin D, Luo D, Lian K, et al. Reconstruction of Traumatic Bone Defect With In Situ Implantation of Dropped Traumatic Segmental Bone Fragments. Orthopedics. 2016;39(1):e14-18. [4] MENG C, YE S, JING J. Masquelet technique combined with flap transplantation for infectious bone and soft tissue defects of lower leg. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34(6):756-760. [5] WANG H, ZHANG Z, WANG W, et al. Scooping Technique to Acquire Cancellous Bone for Grafting in the Masquelet Procedure: A Retrospective Study. Indian J Orthop. 2023;57(8):1267-1275. [6] 薛海鹏,赵勇,刘欣伟,等.膜诱导下髋臼磨钻取骨植骨治疗大段骨缺损患者术后骨吸收发生率及影响因素分析[J].创伤与急危重病医学,2019, 7(2):65-68. [7] DENG AD, INNOCENTI M, ARORA R, et al. Vascularized Small-Bone Transfers for Fracture Nonunion and Bony Defects. Clin Plast Surg. 2020;47(4):501-520. [8] TOROS T, OZAKSAR K. Reconstruction of traumatic tubular bone defects using vascularized fibular graft. Injury. 2021;52(10):2926-2934. [9] YANG HQ, QU L. Ilizarov bone transport technique. Zhongguo Gu Shang. 2022; 35(10):903-907. [10] YANG HQ, ZHANG YH, LI Q, et al. NRD assisted Ilizarov technique in the treatment of infected bone and soft tissue defect of tibia. Zhongguo Gu Shang. 2022;35(10):921-926. [11] MASQUELET AC, FITOUSSI F, BEGUE T, et al. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Hast Esthet. 2000; 45(3):346-353. [12] AYOUBA G, LEMONNE F, KOMBATE NK, et al. Interest of nailing associated with the Masquelet technique in reconstruction of bone defect. J Orthop. 2019;20: 228-231. [13] STAFFORD PR, NORRIS BL. Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: a review of 25 cases. Injury. 2010;41 Suppl 2:S72-77. [14] MESELHY MA, ELHAMMADY AS, SINGER MS. Outcome of Induced Membrane Technique in Treatment of failed previously operated Congenital Pseudarthrosis of the Tibia. Orthop Traumatol Surg Res. 2020;106(5):813-818. [15] KANG Y, WU Y, MA Y, et al. “Primary free-flap tibial open fracture reconstruction with the Masquelet technique” and internal fixation. Injury. 2020;51(12):2970-2974. [16] METSEMAKERS WJ, KUEHL R, MORIARTY TF, et al. Infection after fracture fixation: Current surgical and microbiological concepts. Injury. 2018;49(3):511-522. [17] BLUM AL, BONGIOVANNI JC, MORGAN SJ, et al. Complications associated with distraction osteogenesis for infected nonunion of the femoral shaft in the presence of a bone defect: a retrospective series. J Bone Joint Surg Br. 2010; 92(4):565-570. [18] SALKELD SL, PATRON LP, BARRACK RL, et al. The effect of osteogenic protein-1 on the healing of segmental bone defects treated with autograft or allograft bone. J Bone Joint Surg Am. 2001;83(6):803-816. [19] PALEY D, CATAGNI MA, ARGNANI F, et al. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;(241):146-165. [20] 王月林.创伤性胫骨骨折患者内固定术后骨不连发生的影响因素[J].医药论坛杂志,2021,42(8):112-115. [21] FAOUR O, DIMITRIOU R, COUSINS CA, et al. The use of bone graft substitutes in large cancellous voids: any specific needs. Injury. 2011;42 Suppl 2:S87-90. [22] MORRIS BJ, UNGER RZ, ARCHER KR, et al. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma. 2013;27(9):e196-200. [23] 王波,王斌.创伤性胫骨平台骨折术后切口感染的病原菌分布与影响因素分析[J].海南医学,2020,31(14):1811-1814. [24] 王宇强,贾永森,翟磊,等.骨折内固定术后感染病原菌分布及感染对患者预后的影响[J].中华医院感染学杂志,2017,27(13):3025-3027,3051. [25] 邹璇,徐斌.外固定支架钉道感染的预防与治疗[J].中华医院感染学杂志, 2013,23(5):1075. [26] 蔡成阔,舒衡生.Masquelet技术治疗骨缺损的研究进展[J].中华骨科杂志, 2018,38(3):186-192. [27] GUPTA S, MALHOTRA A, JINDAL R, et al. Role of Beta Tri-calcium Phosphate-based Composite Ceramic as Bone-Graft Expander in Masquelet’s-Induced Membrane Technique. Indian J Orthop. 2019;53(1):63-69. [28] 张一,田晓滨,佘荣峰,等.膜诱导技术结合抗生素硫酸钙颗粒治疗下肢感染性骨缺损[J].中华骨科杂志,2017,37(9):513-519. [29] 李亮,杨海波,米占虎,等.自体微小颗粒骨复合纳米人工骨修复材料治疗感染性骨缺损的疗效分析[J].宁夏医学杂志,2015(1):63-65. [30] 芦北极,孙俊英,王云清,等.ACPC载药核心块状同种异体骨修复长段感染性骨缺损研究[J].现代预防医学,2012,39(8):2011-2012,2017. [31] FENELON M, ETCHEBARNE M, SIADOUS R, et al. Comparison of amniotic membrane versus the induced membrane for bone regeneration in long bone segmental defects using calcium phosphate cement loaded with BMP-2. Mater Sci Eng C Mater Biol Appl. 2021;124:112032. [32] ZHAO Z, WANG G, ZHANG Y, et al. Induced membrane technique combined with antibiotic-loaded calcium sulfate-calcium phosphate composite as bone graft expander for the treatment of large infected bone defects: preliminary results of 12 cases. Ann Transl Med. 2020;8(17):1081. [33] ROUSSET M, WALLE M, CAMBOU L, et al. Chronic infection and infected non-union of the long bones in paediatric patients: preliminary results of bone versus beta-tricalcium phosphate grafting after induced membrane formation. Int Orthop. 2018;42(2):385-393. [34] SASAKI G, WATANABE Y, MIYAMOTO W, et al. Induced membrane technique using beta-tricalcium phosphate for reconstruction of femoral and tibial segmental bone loss due to infection: technical tips and preliminary clinical results. Int Orthop. 2018;42(1):17-24. [35] MORELLI I, DRAGO L, GEORGE DA, et al. Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. 2016;47 Suppl 6:S68-S76. [36] CHENG L, LIN T, KHALAF AT, et al. The preparation and application of calcium phosphate biomedical composites in filling of weight-bearing bone defects. Sci Rep. 2021;11(1):4283. [37] DIAZ MA, BRANCH EA, PAREDES LA, et al. Calcium Phosphate Bone Void Filler Increases Threaded Suture Anchor Pullout Strength: A Biomechanical Study. Arthroscopy. 2020;36(4):1000-1008. [38] ZHANG C, XU G, HAN L, et al. Bone induction and defect repair by true bone ceramics incorporated with rhBMP-2 and Sr. J Mater Sci Mater Med. 2021; 32(9):107. [39] CHO JW, KIM BS, YEO DH, et al. 3D-printed, bioactive ceramic scaffold with rhBMP-2 in treating critical femoral bone defects in rabbits using the induced membrane technique. J Orthop Res. 2021;39(12):2671-2680. [40] ZHOU N, WANG J, LIU C, et al. Clinical application of bioactive CPC loading rhBMP-2 in repairing bone defects. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23(3):257-260. [41] 吴浩俊,谭荣雄,何艳霞,等.磷酸钙活性人工骨与自体骨颗粒环抱式植骨治疗四肢骨不连[J].中国临床解剖学杂志,2020,38(2):202-207. [42] LIM HK, KWON IJ, ON SW, et al. Enhanced Bone Regeneration in Variable-Type Biphasic Ceramic Phosphate Scaffolds Using rhBMP-2. Int J Mol Sci. 2021; 22(21):11485. [43] CONG Y, ZHANG B, FU Y, et al. Recombinant human bone morphogenetic protein 2/porous calcium phosphate cement/autologous bone and combination of platelet-rich plasma in repairing of large bone defects in rabbits by Masquelet technique. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(10):1288-1295. [44] 崔岩,刘志强,吴艳刚.应用两种骨水泥治疗骨质疏松性椎体压缩骨折的骨密度差异[J]. 中国中医骨伤科杂志,2020,28(1):28-34. |
| [1] | Dai Jing, Liu Shasha, Shen Mingjing. Exosome-loaded injectable hydrogel for repairing bone defects around implants [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 347-354. |
| [2] | Xu Yinghua, Liu Jing, You Quan, Wen Zhihao, Gao Lu. Effect of neodymium-doped:yttrium aluminum perovskite laser combined with two kinds of remineralizers on remineralization of early enamel caries [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 360-365. |
| [3] | He Lijun, Qi Xiaojuan. Adipose-derived mesenchymal stem cells overexpressing bone morphogenetic protein 2 promote alveolar bone defect repair in osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 32-37. |
| [4] | Long Guiyue, Li Dongdong, Liao Hongbing. Calcium phosphate cement/poly(lactic-co-glycolic acid) degradation products promote osteoclast differentiation of mouse monocytes [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1193-1198. |
| [5] | Wang Xinjie, Wang Guodong, Zheng Zhongren, Shao Yiming, Wang Jialiang, Ma Hui, Zhao Xiaowei. Manganese-containing bioceramic materials in the field of bone repair [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5570-5576. |
| [6] | Song Meiling, Li Zhengyu, Ai Zizheng, Li Jingna, Zeng Qingfeng, Han Qianqian, Dong Xieping. Repair effect of different hydroxyapatite/beta-tricalcium phosphate coated scaffolds on bone defects [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(30): 4809-4816. |
| [7] | Cui Hongwang, Wang Liangsheng, Wen Peng, Meng Zhibin. Effect of osteoclast TRPV5 channel on in vitro degradation of biological coral artificial bone [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(21): 3337-3342. |
| [8] | Zhao Jinlong, Liu Jichao, Yu Yang. Promoting angiogenesis of platelet-derived growth factor BB modified polycaprolactone and beta-tricalcium phosphate composite scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(21): 3300-3306. |
| [9] | Lu Di, Wan Xinyu, Yang Jinxin, Ding Kexin, Zhang Cheng, Duan Rongquan, Liu Zongxiang. Preparation and osteoinductive properties of tricalcium phosphate ceramics with submicron topology [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(16): 2473-2479. |
| [10] | Xue Peng, Du Bin, Liu Xin, Sun Guangquan, Cheng Tongfei, Chen Hao, He Shuai. Characterization and osteogenic ability of Mg-F membrane/icariin membrane/beta-tricalcium phosphate scaffolds fabricated by coating process combined with 3D printing [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(16): 2480-2487. |
| [11] | Li Jingna, Zeng Qingfeng, Yu Shuyin, Qin Yue, Ai Zizheng, Dong Xieping. Preparation and properties of porous hydroxyapatite scaffolds with biphase calcium phosphate coating [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(16): 2493-2500. |
| [12] | Song Kunxiu, Wang Limin, Ma Rongxing, Hu Yongcheng. Application of patent literature in the study of allogenic demineralized bone matrix [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(14): 2229-2233. |
| [13] | Huang Yanni, Yang Hua, Yang Dongmei, Hu Xulin, Gao Hong, Huang Yina. Rat bone defect repaired with polytrimethylene carbonate/beta-tricalcium phosphate microsphere scaffold [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(12): 1856-1862. |
| [14] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [15] | Yang Sidi, Wang Qian, Xu Nuo, Wang Ronghan, Jin Chuanqi, Lu Ying, Dong Ming. Biodentine enhances the proliferation and differentiation of osteoblasts through upregulating bone morphogenetic protein-2 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 516-520. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||