Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (20): 3143-3149.doi: 10.12307/2024.359
Previous Articles Next Articles
Deferoxamine mesylate improves the repair of jaw bone defects in an ovariectomized rat model of osteoporosis
Tian Ai1, 2, Li Li1, Xiao Tianjiao1, Kang Jiabing1, Zhan Jifan1, Wei Yan1, Chen Helin1, 2
- 1School of Stomatology, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; 2Department of Prosthodontics and Implantology, Affiliated Stomatology Hospital, Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Received:2023-04-20Accepted:2023-06-25Online:2024-07-18Published:2023-09-09 -
Contact:Tian Ai, School of Stomatology, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Prosthodontics and Implantology, Affiliated Stomatology Hospital, Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Tian Ai, MD, Associate professor, Associate chief physician, Master’s supervisor, School of Stomatology, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Prosthodontics and Implantology, Affiliated Stomatology Hospital, Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
Supported by:Guiyang Science and Technology Program Project Fund, No. (2018)1-82 (to TA); National Natural Science Foundation of China, Nos. 81760192 and 82260193 (to TA)
CLC Number:
Cite this article
Tian Ai, Li Li, Xiao Tianjiao, Kang Jiabing, Zhan Jifan, Wei Yan, Chen Helin. Deferoxamine mesylate improves the repair of jaw bone defects in an ovariectomized rat model of osteoporosis[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(20): 3143-3149.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

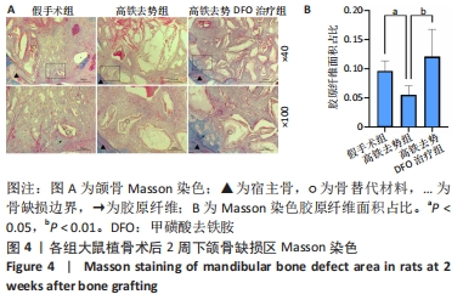
2.4 颌骨苏木精-伊红染色结果 利用苏木精-伊红染色观察早/中时期骨缺损区炎性细胞浸润及新骨生成情况。由图3可见,植骨术后2周时,3组骨缺损边缘与颗粒材料间均可见大量炎症细胞浸润,与假手术组相比,高铁去势组炎症细胞更多,未见明显新骨基质生成;与高铁去势组相比,高铁去势DFO治疗组见较少的炎症细胞浸润,少量新生骨基质,在骨质周围可见大量排列成单层、形状不规则胞质深染的成骨细胞,新生骨质与基骨组织相延续,界限模糊。植骨术后12周时,假手术组骨缺损边界处见新生骨质;与假手术组相比,高铁去势组仅边界处见少量条索状骨小梁结构,稀疏分布,未能连接成片,矿化程度与假手术组比较明显降低。而高铁去势DFO治疗组骨缺损边界及中央区域形成多个片状骨化中心,骨小梁分布致密,骨质矿化程度与正常骨接近,新骨生成的质与量较高铁去势组明显提高。"

| [1] Management of Osteoporosis in Postmenopausal Women: The 2021 Position Statement of The North American Menopause Society’’ Editorial Panel. Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society. Menopause. 2021;28(9):973-997. [2] TAO ZS, LI TL, WEI S. Silymarin prevents iron overload induced bone loss by inhibiting oxidative stress in an ovariectomized animal model. Chem Biol Interact. 2022;366:110168. [3] LU M, LIU Y, SHAO M, et al. Associations of Iron Intake, Serum Iron and Serum Ferritin with Bone Mineral Density in Women: The National Health and Nutrition Examination Survey, 2005-2010. Calcif Tissue Int. 2020;106(3): 232-238. [4] BAJBOUJ K, SHAFARIN J, ALLAM H, et al. Elevated Levels of Estrogen Suppress Hepcidin Synthesis and Enhance Serum Iron Availability in Premenopausal Women. Exp Clin Endocrinol Diabetes. 2018;126(7):453-459. [5] HUANG X, XU Y, PARTRIDGE NC. Dancing with sex hormones, could iron contribute to the gender difference in osteoporosis? Bone. 2013;55(2):458-460. [6] ZIMMERMANN MB, HURRELL RF. Nutritional iron deficiency. Lancet. 2007; 370(9586):511-520. [7] LI GF, PAN YZ, SIROIS P, et al. Iron homeostasis in osteoporosis and its clinical implications. Osteoporos Int. 2012;23(10):2403-2408. [8] XUE Y, YANG J, LUO J, et al. Disorder of Iron Metabolism Inhibits the Recovery of Unloading-Induced Bone Loss in Hypomagnetic Field. J Bone Miner Res. 2020;35(6):1163-1173. [9] GAUDIO A, MORABITO N, CATALANO A, et al. Pathogenesis of Thalassemia Major-associated Osteoporosis: A Review with Insights from Clinical Experience. J Clin Res Pediatr Endocrinol. 2019;11(2):110-117. [10] XU S, ZHANG G, GUO JF, et al. Associations between osteoporosis and risk of periodontitis: A pooled analysis of observational studies. Oral Dis. 2021;27(2):357-369. [11] HONG SJ, YANG BE, YOO DM, et al. Analysis of the relationship between periodontitis and osteoporosis/fractures: a cross-sectional study. BMC Oral Health. 2021;21(1):125. [12] DREYER H, GRISCHKE J, TIEDE C, et al. Epidemiology and risk factors of peri-implantitis: A systematic review. J Periodontal Res. 2018;53(5):657-681. [13] LIU LN, ZHANG XH, LIU HH, et al. Osteogenesis Differences Around Titanium Implant and in Bone Defect Between Jaw Bones and Long Bones. J Craniofac Surg. 2020;31(8):2193-2198. [14] OLEJNIK C, FALGAYRAC G, DURING A, et al. Doses effects of zoledronic acid on mineral apatite and collagen quality of newly-formed bone in the rat’s calvaria defect. Bone. 2016;89:32-39. [15] LIN W, LI Q, ZHANG D, et al. Mapping the immune microenvironment for mandibular alveolar bone homeostasis at single-cell resolution. Bone Res. 2021;9(1):17. [16] CHEN B, YAN YL, LIU C, et al. Therapeutic effect of deferoxamine on iron overload-induced inhibition of osteogenesis in a zebrafish model. Calcif Tissue Int. 2014;94(3):353-360. [17] 陈爱华,赵国阳,庄琴,等.去铁胺对输血相关性铁过载患者骨密度的影响[J].中国骨质疏松杂志,2018,24(3):311-314. [18] 郑妮娜,卢俊玲,盛慧.甲磺酸去铁胺辅助治疗绝经后骨质疏松症的可行性和安全性研究[J].中国骨质疏松杂志,2019,25(7):998-1001. [19] LIU Y, LIU J, CAI F, et al. Hypoxia During the Consolidation Phase of Distraction Osteogenesis Promotes Bone Regeneration. Front Physiol. 2022;13:804469. [20] 杜文瑜,杨静文,姜婷.甲磺酸去铁胺促进大鼠颅骨临界骨缺损血管化骨再生的早期连续观察[J].北京大学学报(医学版),2021,53(6):1171-1177. [21] HOLDEN P, NAIR LS. Deferoxamine: An Angiogenic and Antioxidant Molecule for Tissue Regeneration. Tissue Eng Part B Rev. 2019;25(6):461-470. [22] LANE JM, RUSSELL L, KHAN SN. Osteoporosis. Clin Orthop Relat Res. 2000; (372):139-150. [23] GUIGLIA R, DI FEDE O, LO RUSSO L, et al. Osteoporosis, jawbones and periodontal disease. Med Oral Patol Oral Cir Bucal. 2013;18(1):e93-99. [24] WANG B, FENG C, LIU Y, et al. Recent advances in biofunctional guided bone regeneration materials for repairing defective alveolar and maxillofacial bone: A review. Jpn Dent Sci Rev. 2022;58:233-248. [25] MARDAS N, BUSETTI J, DE FIGUEIREDO JA, et al. Guided bone regeneration in osteoporotic conditions following treatment with zoledronic acid. Clin Oral Implants Res. 2017;28(3):362-371. [26] YOUSEFZADEH N, KASHFI K, JEDDI S, et al. Ovariectomized rat model of osteoporosis: a practical guide. EXCLI J. 2020;19:89-107. [27] WANG Z, DUAN R, JIN Y, et al. Effects of ferric ammonium citrate on iron accumulation, bone turnover and bone density in ovariectomized rat models with osteoporosis. Cell Mol Biol (Noisy-le-grand). 2022;68(8):163-166. [28] ZHANG C, MENG T, DAN Z, et al. Minocycline ameliorates osteoporosis induced by ovariectomy (OVX) and iron accumulation via iron chelation, bone metabolism regulation and inhibition of oxidative stress. QJM. 2020: hcaa271. doi: 10.1093/qjmed/hcaa271. [29] DÍAZ-CASTRO J, LÓPEZ-FRÍAS MR, CAMPOS MS, et al. Severe nutritional iron-deficiency anaemia has a negative effect on some bone turnover biomarkers in rats. Eur J Nutr. 2012;51(2):241-247. [30] TAO H, GE G, LIANG X, et al. ROS signaling cascades: dual regulations for osteoclast and osteoblast. Acta Biochim Biophys Sin (Shanghai). 2020; 52(10):1055-1062. [31] BALOGH E, PARAGH G, JENEY V. Influence of Iron on Bone Homeostasis. Pharmaceuticals (Basel). 2018;11(4):107. [32] ZANDI M, DEHGHAN A, GHEYSARI F, et al. Evaluation of teriparatide effect on healing of autografted mandibular defects in rats. J Craniomaxillofac Surg. 2019;47(1):120-126. [33] ZHAO J, HU J, WANG S, et al. Combination of beta-TCP and BMP-2 gene-modified bMSCs to heal critical size mandibular defects in rats. Oral Dis. 2010;16(1):46-54. [34] 高超.甲磺酸去铁胺对去势小鼠、大鼠骨质疏松模型影响的实验研究[D].苏州:苏州大学,2013. [35] 刘江锋.低氧模拟剂对膝关节置换术后钛假体骨整合影响和术前骨质疏松、骨代谢指标及危险因素的相关研究[D].石家庄:河北医科大学,2022. [36] ZHANG J, HU W, DING C, et al. Deferoxamine inhibits iron-uptake stimulated osteoclast differentiation by suppressing electron transport chain and MAPKs signaling. Toxicol Lett. 2019;313:50-59. [37] ZHANG J, ZHAO H, YAO G, et al. Therapeutic potential of iron chelators on osteoporosis and their cellular mechanisms. Biomed Pharmacother. 2021;137:111380. [38] JIANG Z, WANG H, QI G, et al. Iron overload-induced ferroptosis of osteoblasts inhibits osteogenesis and promotes osteoporosis: An in vitro and in vivo study. IUBMB Life. 2022;74(11):1052-1069. [39] JIA P, CHEN H, KANG H, et al. Deferoxamine released from poly(lactic-co-glycolic acid) promotes healing of osteoporotic bone defect via enhanced angiogenesis and osteogenesis. J Biomed Mater Res A. 2016;104(10): 2515-2527. [40] 苏州大学. 甲磺酸去铁胺在制备治疗绝经后骨质疏松疾病药物中的用途:CN201110437117.2[P]. 2012-07-04. |
| [1] | Yang Yufang, Yang Zhishan, Duan Mianmian, Liu Yiheng, Tang Zhenglong, Wang Yu. Application and prospects of erythropoietin in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1443-1449. |
| [2] | Guo Sutong, Feng Dehong, Guo Yu, Wang Ling, Ding Yujian, Liu Yi, Qian Zhengying, Li Mingyang. Construction and finite element analysis of normal and osteoporotic hip models [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1342-1346. |
| [3] | Zhang Xiaoyun, Liu Hua, Chai Yuan, Chen Feng, Zeng Hao, Gao Zhengang, Huang Yourong. Effect of Yishen Gushu Formula on bone metabolic markers and clinical efficacyn in patients with osteoporosis of kidney deficiency and blood stasis type [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1155-1160. |
| [4] | Dai Yuexing, Zheng Liqin, Wu Minhui, Li Zhihong, Li Shaobin, Zheng Desheng, Lin Ziling. Effect of vessel number on computational fluid dynamics in vascular networks [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1206-1210. |
| [5] | Wang Shanshan, Shu Qing, Tian Jun. Physical factors promote osteogenic differentiation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1083-1090. |
| [6] | Zhang Min, Peng Jing, Zhang Qiang, Chen Dewang. Mechanical properties of L3/4 laminar decompression and intervertebral fusion in elderly osteoporosis patients analyzed by finite element method [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 847-851. |
| [7] | Xue Xiaofeng, Wei Yongkang, Qiao Xiaohong, Du Yuyong, Niu Jianjun, Ren Lixin, Yang Huifeng, Zhang Zhimin, Guo Yuan, Chen Weiyi. Finite element analysis of osteoporosis in proximal femur after cannulated screw fixation for femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 862-867. |
| [8] | Kaiyisaier•Abudukelimu, Maimaitimin•Abulimiti, Li Lei, Yang Xiaokai, Zhang Yukun, Liu Shuai. Effect of lumbar CT values in the diagnosis of osteoporosis in women patients with lumbar degenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 945-949. |
| [9] | Wang Liping, Lian Tianxing, Hu Yongrong, Yang Hongsheng, Zeng Zhimou, Liu Hao, Qu Bo. HU value of chest CT vertebral body in the opportunistic screening of type 2 diabetes mellitus osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 950-954. |
| [10] | Lan Weiwei, Yu Yaodong, Huang Di, Chen Weiyi. In vitro degradation behavior of Mg-Zn-Ca alloys [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 717-723. |
| [11] | Zhou Xiaowen, Fu Zuchang, Huang Fei, Ai Jianguo, Zhao Feng. Bone defect blocked by bone cement segmental filling in single-plane tibial bone transport [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 736-740. |
| [12] | Yu Zhaoyu, Tan Lixin, Sun Kai, Lu Yao, Li Yong. Meta-analysis of cement-augmented pedicle screw for thoracolumbar degenerative diseases with osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 813-820. |
| [13] | Wei Yuanxun, Chen Feng, Lin Zonghan, Zhang Chi, Pan Chengzhen, Wei Zongbo. The mechanism of Notch signaling pathway in osteoporosis and its prevention and treatment with traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 587-593. |
| [14] | Yang Yuqing, Chen Zhiyu. Role and application of early transient presence of M1 macrophages in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 594-601. |
| [15] | Zhou Shibo, Guan Jianbin, Yu Xing, Zhao He, Yang Yongdong, Liu Tao. Animal models of femoral bone defects: preparation status and characteristics [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 633-638. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||