[1] CHEN Y, ZHAO G, LI N, et al. Role of 4‑aminobutyrate aminotransferase (ABAT) and the lncRNA co‑expression network in the development of myelodysplastic syndrome. Oncol Rep. 2019;42(2):509-520.
[2] BEWERSDORF JP, ZEIDAN AM. Risk-Adapted, Individualized Treatment Strategies of Myelodysplastic Syndromes (MDS) and Chronic Myelomonocytic Leukemia (CMML). Cancers (Basel). 2021;13(7):1610.
[3] MENSSEN AJ, WALTER MJ. Genetics of progression from MDS to secondary leukemia. Blood. 2020;136(1):50-60.
[4] CAZZOLA M, DELLA PORTA MG, MALCOVATI L. The genetic basis of myelodysplasia and its clinical relevance. Blood. 2013;122(25):4021-4034.
[5] KULASEKARARAJ AG, MOHAMEDALI AM, MUFTI GJ. Recent advances in understanding the molecular pathogenesis of myelodysplastic syndromes. Br J Haematol. 2013;162(5):587-605.
[6] MÉNDEZ-FERRER S, BONNET D, STEENSMA DP, et al. Bone marrow niches in haematological malignancies. Nat Rev Cancer. 2020;20(5):285-298.
[7] MIAN SA, BONNET D. Nature or Nurture? Role of the Bone Marrow Microenvironment in the Genesis and Maintenance of Myelodysplastic Syndromes. Cancers (Basel). 2021;13(16):4116.
[8] WANG C, YANG Y, GAO S, et al. Immune dysregulation in myelodysplastic syndrome: Clinical features, pathogenesis and therapeutic strategies. Crit Rev Oncol Hematol. 2018;122:123-132.
[9] XU B, HU R, LIANG Z, et al. Metabolic regulation of the bone marrow microenvironment in leukemia. Blood Rev. 2021;48:100786.
[10] VADAKEKOLATHU J, MINDEN MD, HOOD T, et al. Immune landscapes predict chemotherapy resistance and immunotherapy response in acute myeloid leukemia. Sci Transl Med. 2020;12(546):eaaz0463.
[11] TETTAMANTI S, PIEVANI A, BIONDI A, et al. Catch me if you can: how AML and its niche escape immunotherapy. Leukemia. 2022;36(1):13-22.
[12] KITTANG AO, KORDASTI S, SAND KE, et al. Expansion of myeloid derived suppressor cells correlates with number of T regulatory cells and disease progression in myelodysplastic syndrome. Oncoimmunology. 2015;5(2):e1062208.
[13] HAFERLACH C, BACHER U, KOHLMANN A, et al. CDKN1B, encoding the cyclin-dependent kinase inhibitor 1B (p27), is located in the minimally deleted region of 12p abnormalities in myeloid malignancies and its low expression is a favorable prognostic marker in acute myeloid leukemia. Haematologica. 2011;96(6):829-836.
[14] 张艳,邱镜滢,何琦,等.31例12p染色体畸变血液病患者细胞遗传学和临床分析[J].中国实验血液学杂志,2004,12(2):166-169.
[15] GONZALEZ-APARICIO M, ALFARO C. Significance of the IL-8 pathway for immunotherapy. Hum Vaccin Immunother. 2020;16(10):2312-2317.
[16] TEIJEIRA A, GARASA S, OCHOA MC, et al. IL8, Neutrophils, and NETs in a Collusion against Cancer Immunity and Immunotherapy. Clin Cancer Res. 2021;27(9):2383-2393.
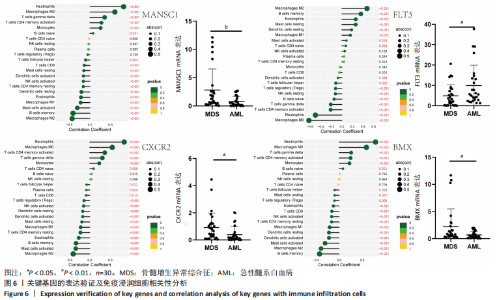
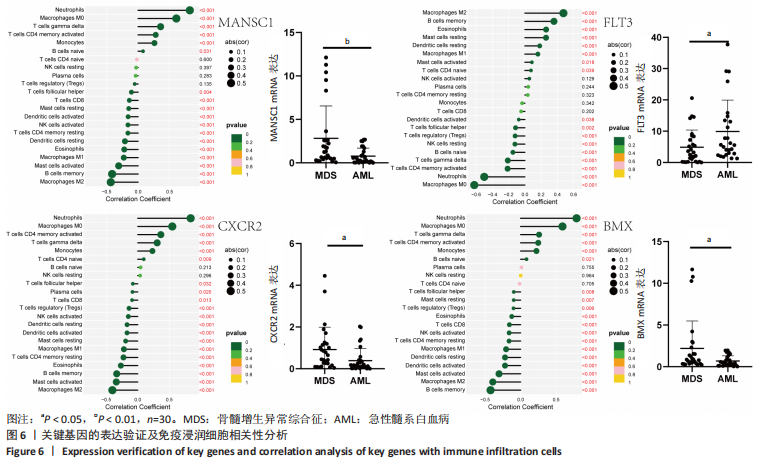
[17] WANG L, ZHANG YL, LIN QY, et al. CXCL1-CXCR2 axis mediates angiotensin II-induced cardiac hypertrophy and remodelling through regulation of monocyte infiltration. Eur Heart J. 2018;39(20):1818-1831.
[18] ZHANG W, WANG H, SUN M, et al. CXCL5/CXCR2 axis in tumor microenvironment as potential diagnostic biomarker and therapeutic target. Cancer Commun (Lond). 2020;40(2-3):69-80.
[19] CENNI B, GUTMANN S, GOTTAR-GUILLIER M. BMX and its role in inflammation, cardiovascular disease, and cancer. Int Rev Immunol. 2012;31(2):166-173.
[20] BUELOW DR, BHATNAGAR B, ORWICK SJ, et al. BMX kinase mediates gilteritinib resistance in FLT3-mutated AML through microenvironmental factors. Blood Adv. 2022;6(17):5049-5060.
[21] DAVER N, SCHLENK RF, RUSSELL NH, et al. Targeting FLT3 mutations in AML: review of current knowledge and evidence. Leukemia. 2019; 33(2):299-312.
[22] CUETO FJ, SANCHO D. The Flt3L/Flt3 Axis in Dendritic Cell Biology and Cancer Immunotherapy. Cancers (Basel). 2021;13(7):1525.
[23] WILSON KR, VILLADANGOS JA, MINTERN JD. Dendritic cell Flt3 - regulation, roles and repercussions for immunotherapy. Immunol Cell Biol. 2021;99(9):962-971. |