Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (10): 1604-1609.doi: 10.12307/2022.210
Previous Articles Next Articles
Influence of surface treatment technology on friction and wear performance of artificial joints
Liu Zhiqiang, Liang Yuyao, Gao Ge, Meng Shun, Xie Zhongqi, Su Yu
- Jiangsu University of Science and Technology, Zhenjiang 212100, Jiangsu Province, China
-
Received:2020-11-21Revised:2020-11-27Accepted:2020-12-19Online:2022-04-08Published:2021-10-27 -
Contact:Liu Zhiqiang, Associate professor, Master’s supervisor, Jiangsu University of Science and Technology, Zhenjiang 212100, Jiangsu Province, China -
About author:Liu Zhiqiang, MD, Associate professor, Master’s supervisor, Jiangsu University of Science and Technology, Zhenjiang 212100, Jiangsu Province, China
CLC Number:
Cite this article
Liu Zhiqiang, Liang Yuyao, Gao Ge, Meng Shun, Xie Zhongqi, Su Yu. Influence of surface treatment technology on friction and wear performance of artificial joints[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1604-1609.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

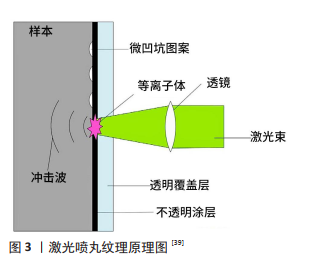
人工关节使用寿命的主要评价指标是摩擦系数和磨损 率[20],减少摩擦磨损是提高人工关节质量和延长使用寿命的最佳途径[21-22]。有研究表明,较低的表面粗糙度可以获得较好的表面润湿性,从而有效提高人工关节的摩擦磨损性能[23]。 2.1 表面纹理技术 大量研究结果表明,摩擦接触表面并不是越光滑其摩擦磨损性能越好,与光滑表面相比,带有纹理的表面具有更加稳定的摩擦磨损性能。表面纹理技术通过改变人工关节表面微结构改善润滑膜的厚度、减少接触面积,最终实现减少人工关节表面的摩擦磨损[24]。不同的表面纹理结构对人工关节表面的摩擦磨损性能会产生不同的影响,在表面纹理结构中槽纹、脊纹和凹坑是应用最多的结构[25]。CHOUDHURY等[20]以不同材料的人工关节为研究对象,分别探究了不同凹坑结构对人工关节摩擦系数和表面性能的影响。SAWANO等[26]指出,在人工关节表面制备的微凹坑可以降低金属对超高分子量聚乙烯的磨损,延长人工关节的使用寿命。 表面纹理技术主要包括机械加工、离子束纹理、激光处理、喷砂、电抛光和化学腐蚀等,这些技术通过在材料表面形成微结构特征来改变人工关节的表面性能。 2.1.1 激光表面纹理技术 激光表面纹理技术可以有效提高人工关节的摩擦磨损性能,延长其使用寿命,深受研究者的关注[27]。XU等[28]受鱼鳞和虾的表面重叠结构形态的启发,在Ti6Al4V合金植入体表面通过激光纹理技术制备重叠形态结构,并通过实验验证了该结构可以提高植入体表面的摩擦特性。TIAINEN等[25]比较了不同激光纹理结构对钛合金植入体润湿性能和摩擦性能的影响。脉冲激光微加工已成为目前国内外研究的热点之一,根据单个脉冲持续时间的长短可以将脉冲激光分为纳秒激光、飞秒激光和皮秒激光等。纳秒激光加工具有低成本和较高效率的优点,但成型件存在质量较差、残渣较多、光洁度较低的不足;飞秒激光加工具有加热速度快、热影响区小、成型精度高的优势,但也存在使用成本高的劣势;与纳秒激光加工相比,皮秒激光加工的成型件质量较高、残渣较少、热影响区较小,同时相对于飞秒激光加工而言,皮秒激光加工具有成本效益更高、性能更可靠的优点。AHUIR-TORRES等[29]利用皮秒激光在铝合金表面分别制备了微凹坑和十字槽纹结构,研究激光纹理对铝合金润湿性的影响。ARENAS等[30]采用固态皮秒脉冲激光器在Ti6Al4V合金表面制备不同角度的菱形花纹纹理,利用双向滑动磨损试验进一步研究其摩擦磨损性能。激光表面纹理技术具有适应性强、精度高、效率高等特点,但采用该技术制备的微纹理结构的粗糙度会高于基底的初始粗糙度[31]。 2.1.2 机械加工 机械加工是通过将基材加工区域的材料去除或提取的方法来制备表面纹理结构,常用的机械加工技术有数控加工、珩磨、磨削、抛光等。不同的制备方法对材料表面的摩擦磨损性能有不同的影响。有研究采用微型数控机械技术制备表面微凹坑结构,当其密度为10%时材料表面的摩擦系数只有光滑表面的1/2。ROY等[32]采用数控微钻床在陶瓷基板上制备了微凹坑结构,并研究了微凹坑结构的摩擦性能,发现当微凹坑的面积密度为15%时,陶瓷基板减少了22%的摩擦和53%的磨损量。CHYR等[33]的研究发现,通过五轴铣床在CoCr合金股骨表面上制备微纹理结构可以明显减少接触表面之间的摩擦发热和摩擦损失。CHOUDHURY等[34]的研究发现,在模拟髋关节运动实验中珩磨法处理的表面平均摩擦系数降低了50%,磨损率下降了38%。 2.1.3 其他技术 人工关节可以采用不同的表面技术进行处理。电火花加工处理技术也是表面处理技术的一种,该技术可以改善合金的表面硬度和摩擦磨损性能。喷丸强化技术是对疲劳使用寿命有着积极影响的技术,该技术被广泛应用于钛及其合金的最终表面处理技术[35]。虽有文献指出电火花加工技术、化学铣削技术和喷丸强化技术是有益的表面处理技术,但是很少有研究者对这3种技术的结合应用进行探究,于是HAVLIKOVA等[36]提出了新型表面处理方法即将3种技术结合应用,可以降低电火花加工处理对Ti6Al4V合金产生的表面整体粗糙度。 不同的表面处理方法对人工关节摩擦磨损性能有着不同的意义。HE等[37]结合激光表面纹理技术和磁控溅射技术在钛合金表面制备了不同密度的微凹痕和类金刚石涂层,当类金刚石涂层的凹痕面积密度为44%时钛合金基体的耐摩性能显著提高。在摩擦表面上制备凹凸纹理可显著提高人工关节的润滑和耐久性能。ITO等[38]为测定人工髋关节摩擦表面形成的凹痕是否能降低超高分子量聚乙烯磨损,在CoCr合金股骨头上采用放电蚀刻技术制作圆形凹痕,通过实验证明了这些凹痕可以明显降低超高分子质量聚乙烯的摩擦系数。激光喷丸纹理是以激光加工为基础,结合喷丸处理技术的一种新型表面纹理技术,图3为其原理图[39]。电子束纹理是一种很有发展前景的表面处理技术,该技术可以在Ti6Al4V合金表面制备纹理结构图案,用以改善合金表面的摩擦学性能[40]。 在现有研究中,已有很多实验证明了表面纹理技术对提高人工关节摩擦磨损性能有着重要的意义,但是在不同的研究中研究者对实验样品所施加的荷载是不同的,在不同载荷条件下评估表面纹理技术对人工关节摩擦磨损性能的影响具有一定的难度。有研究人员提出,可以将表面纹理技术与表面涂层技术相结合用来提高人工关节表面性能。类金刚石涂层具有良好的摩擦学特性和一些类似金刚石的性能,被广泛应用于人工关节表面。最近的研究表明,在类金刚石涂层表面制备表面纹理可以提高植入材料的耐磨性[21]。CHOUDHURY等[41]指出在纹理表面涂覆类金刚石涂层,一方面可以降低表面摩擦系数,另一方面带有纹理的表面在接触面之间可提供液体流动时的动力流,以此来改善润滑效果。 2.2 表面涂层技术 表面涂层主要具有保护、装饰和功效作用,可改善人工关节表面性能、提高人工关节的使用寿命[42]。常用的表面涂层技术有:等离子喷涂、阳极氧化、微弧氧化、溶胶-凝胶法、电化学沉积、热喷涂法、离子注入法、物理气相沉积和化学气相沉积等[43]。 2.2.1 物理气相沉积 物理气相沉积作为表面涂层技术中研究最为普遍的技术,它包含了许多子类,如:磁控溅射、离子束沉积、电子束辅助沉积、脉冲等离子体沉积和电弧气相沉积等方法[44-45]。 在大多数情况下,金属股骨头与超高分子质量聚乙烯髋臼杯连接在一起使用的状态是良好的,但在一些情况下金属股骨头会导致软股骨头的磨损,造成人工关节无菌松动,最终导致人工关节的失效。针对这种情况,许多研究者提出在金属股骨头上沉积TiN、CrN或类金刚石等硬陶瓷涂层,用来降低超高分子质量聚乙烯的磨损率。 自从1980年来,基于物理气相沉积技术沉积的TiN涂层是在全髋关节置换术中最常用的涂层[46]。物理气相沉积技术制备的涂层具有较好的耐磨性,有实验证明TiN涂层涂覆的Ti6Al4V合金股骨头比老一代髋关节的耐磨性更好[47]。表面涂层的摩擦系数是最受关注的因素之一,许多研究者在涂覆一层或两层涂层之后得到的摩擦系数略低,但仍高于0.1。ZUO等[48]对TiN涂层的摩擦系数进行了深入研究。单独的物理气相沉积技术在低硬度的基底沉积涂层时,其摩擦学性能具有一定的局限性,会导致涂层的断裂和分层,MARIN等[49]提出基于扩散处理的混合工艺,用以提高物理气相沉积涂层的整体耐蚀性。氮化物涂层、碳化物涂层、氧化铝涂层和ZrO2涂层是股骨头常用的生物惰性陶瓷涂层,这些涂层在使用中会分层,易导致超高分子质量聚乙烯磨损加剧。TiCuN涂层的硬度可以通过掺杂少量的铜来提高[50],有实验结果显示,电弧离子镀技术制备的质量分数5.2%Cu的TiCuN涂层与纯锡和锡/铜纳米复合涂层相比具有更高的硬度、更低的摩擦系数和更强的耐磨性[16]。MULLIGAN等[51]采用电子束辅助电弧离子镀技术制备TiCuN涂层,实验结果表明掺杂的Cu含量对涂层的硬度有重要影响,只有当Cu掺杂量不超过2%-3%时TiCuN涂层才能获得较高的硬度。除了金属元素Cu可以改善涂层的摩擦学特性之外,Ag也可以改善涂层的摩擦磨损性能。KSTENBAUER 等[52]用磁控管共溅射技术制备了TiN/Ag复合涂层,证实了银可以降低涂层的摩擦磨损。 耐久性被认为是涂层的主要缺点,在没有润滑剂的情况下,物理气相沉积技术制备的涂层会发生剥落或降解情况[28]。电子束辅助沉积已经被实践用于物理气相沉积涂层可获得高致密和高耐磨性的涂层[44]。利用等离子体辅助电子束物理气相沉积技术在Ti6Al4V合金基底上沉积TiN涂层,可以进一步提高涂层的磨损性能和腐蚀性能[53]。 2.2.2 溶胶-凝胶法 溶胶-凝胶技术是物理沉积技术的一种补充,该技术沉积的涂层具有独特的特征,如柔韧性、形态结构可控制性、机械性能等[44]。溶胶-凝胶技术可以在不同基底材料上沉积不同成分和特性的涂层,当沉积羟磷灰石复合涂层时可以观察到羟磷灰石复合涂层与基底的结合强度显著提高[42]。采用溶胶-凝胶技术制备的含银羟基磷灰石涂层,不仅能够促进人体成骨细胞的增殖与分化,而且能够增强人工关节的抗菌性能。BALLARRE等[54]指出溶胶-凝胶技术制备的生物涂层,可以作为提高316L不锈钢体内性能的一种潜在解决方案。但值得注意的是,采用溶胶-凝胶技术制备涂层时,若干燥过程中凝胶收缩大则易产生大量的裂纹,当裂纹出现在基底上时可以制备多层涂层来修补,但裂纹出现在表面则无法避免。 2.2.3 化学气相沉积 相对于物理气相沉积技术而言,化学气相沉积技术需要更高的操作温度和更大的步长覆盖。化学气相沉积技术具有灵活的几何纹理特征,可形成致密且均匀的涂层,且与基体的结合牢固,涂层的质量也相对稳定[28,44],但研究过程中选择沉积材料和基底材料时需要具备丰富的化学知识底蕴。TARNOWSKI等[55]研究发现,碳层对降低聚醚醚酮及其衍生物复合材料与氮化钛合金之间的摩擦系数具有积极的影响。在超高分子质量聚乙烯上采用电子回旋共振微波等离子体化学气相沉积a-C:H涂层,可以显著改善其耐磨性和抗划伤性[56]。等离子增强化学气相沉积技术具有物理气相沉积技术和化学气相沉积技术的优点,采用该技术在金属材料表面制备氮化钛涂层可以显著改善金属材料表面的摩擦性能。采用射频等离子体增强化学气相沉积技术在基材表面制备的类金刚石涂层,不仅具有优异的力学性能,而且随着涂层厚度的增加,涂层的表面粗糙度减小,涂层与基材接触面的结合强度提高。 2.2.4 等离子喷涂技术 与物理气相沉积技术和化学气相沉积技术相比,等离子喷涂技术所需的温度更高、沉积的涂层更厚[44]。等离子体喷涂技术主要通过提高材料表面硬化程度进而改善材料的疲劳强度、耐磨性和承载能。?óRAWSKI等[57]以等离子喷涂技术中的喷涂参数为研究对象,深入研究了喷涂参数对摩擦系数、硬度和表面粗糙度的影响。研究人员发现,采用等离子喷涂技术制备的Al2O3涂层具有表面硬度较高、粗糙度较低、孔隙率较小、抗磨性更佳的优势。与烧结技术制备的涂层相比,等离子喷涂技术制备的涂层具有更高的硬度和更好的耐磨性。等离子喷涂技术制备的羟磷灰石和羟基磷灰石-碳钠米管涂层表面具有较高的粗糙度、较小的接触面积,减少了在磨损过程中质量和体积的损失量[58]。在Ti6Al4V合金上涂覆的羟磷灰石涂层可以提高Ti6Al4V合金的抗弹塑性变形能力[59]。但等离子喷涂技术存在涂层不均匀、羟磷灰石涂层易出现裂纹、高温下羟磷灰石涂层易分解等不足[60]。为了解决羟磷灰石与基底之间的分层问题,有研究应用等离子涂层技术制备了一种复合涂层,用于改善羟磷灰石涂层与基底之间的连接。 2.2.5 离子注入技术 离子注入技术对增强涂层的耐磨性、硬度和抗接触疲劳性能具有积极的意义[61]。其中碳离子的注入对CoCrMo合金的硬度、磨损量和摩擦均具有显著影 响[62]。氮离子注入后的CoCrMo合金,表面耐磨性和基体硬度会显著提高,经过磨损试验后发现氮离子注入和氮化硼涂覆后的CoCrMo合金与超高分子质量聚乙烯之间的的磨损率显著降低了48%[63]。氮离子注入与氮化硼涂层相结合的方法为延长金属聚合物人工关节寿命提供了新思路。 NAVINSEK等[64]指出在合金表面先注入钛和钽离子再注入氮等离子体,可获得低摩擦和高耐磨的表面性能。在316L不锈钢表面采用等离子浸没离子注入方法沉积锡涂层后,人工关节中超高分子质量聚乙烯磨损的降低具有显著效果。当采用离子注入法对Ti6Al4V合金进行处理后,得到的钛合金与超高分子质量聚乙烯之间的摩擦显著减少。离子注入法对人工关节材料的摩擦磨损性能具有显著的改善效果,但其主要缺点是溶液中金属离子的释放会加剧和表面涂层厚度不足。 2.2.6 其他技术 表面氧化技术对改善人工关节的表面性能有重要意义,用ZrO2、Al2O3和碳化硅等材料对聚醚醚酮进行填充改性可以使聚醚醚酮人工关节满足更高的制造和性能要求[65]。在人工关节表面涂层的应用中,聚醚醚酮及其复合涂层的应用和摩擦磨损性能研究并不广泛,但有研究表明,当对聚醚醚酮涂层填充质量分数5%的ZrO2时,涂层具有最好的摩擦学性能[66]。Al2O3陶瓷是股骨头常用的生物材料,该材料虽具有较高的耐磨性,但当承受较大负载时人工关节易发生断裂[67]。在钛合金表面通过传统的铝沉积技术无法氧化产生足够厚而致密的氧化铝层,冷喷涂技术和微弧氧化技术的结合实现了在钛合金表面上制备出厚而致密的氧化铝层。微弧氧化技术结合了电化学氧化和高压火花处理技术,可以在铝及其合金表面产生厚而致密且高硬度的氧化铝层[68],该技术工艺简单,可以制备具有较高耐磨性和耐腐蚀性的涂层,但工艺参数及配套设备的研究还存在一定的不足。"
| [1] SHEN G, FANG F, KANG C. Tribological Performance of Bioimplants: A Comprehensive Review. Nanotechnol Precis Eng. 2018;1(2):107-122. [2] SHEN G, ZHANG JF, FANG FZ. In Vitro Evaluation of Artificial Joints: A Comprehensive Review. Adv Manufact. 2019;7:1-14. [3] MATTEI L, Di PUCCIO F, PICCIGALLO B, et al. Lubrication and wear modelling of artificial hip joints: A review. Tribol Int. 2011;44(5): 532-549. [4] VOUTAT C, NOHAVA J, WANDEL J, et al. The Dynamic Friction Coefficient of the Wet Bone-Implant Interface: Influence of Load, Speed, Material and Surface Finish. Biotribology. 2019;17:64-74. [5] WANG C, ZHANG GQ, LI Z, et al. Tribological behavior of Ti-6Al-4V against cortical bone in different biolubricants. J Mech Behav Biomed Mater. 2019;90:460-471. [6] GRANT JA, BISHOP NE, GOTZEN N, et al. Artificial composite bone as a model of human trabecular bone: the implant-bone interface. J Biomech. 2007;40(5):1158-1164. [7] GERINGER J, ATMANI F, FOREST B. Friction–corrosion of AISI 316L/bone cement and AISI 316L/PMMA contacts: Ionic strength effect on tribological behaviour. Wear. 2009;267(5):763-769. [8] DAMM NB, MORLOCK MM, BISHOP NE. Friction coefficient and effective interference at the implant-bone interface. J Biomech. 2015; 48(12):3517-3521. [9] GUO Y, HAO ZX, WAN C. Tribological characteristics of polyvinylpyrrolidone (PVP) as a lubrication additive for artificial knee joint. Tribol Int. 2016;93:214-219. [10] HUSSAIN O, SALEEM SS, AHMAD B. Friction and wear performance evaluation of UHMWPE using Taguchi based grey approach: A study on the influence of load and bio-serum lubrication. Mater Chem Phys. 2020;239:121918. [11] CUI W, BIAN Y, ZENG H, et al. Structural and tribological characteristics of ultra-low-wear polyethylene as artificial joint materials. J Mech Behav Biomed Mater. 2020;104:103629. [12] NAKANISHI Y, NAKASHIMA Y, FUJIWARA Y, et al. Influence of surface profile of Co-28Cr-6Mo alloy on wear behaviour of ultra-high molecular weight polyethylene used in artificial joint. Tribol Int. 2018;118: 538-546. [13] RAN QC, YANG WH, HU Y, et al. Osteogenesis of 3D printed porous Ti6Al4V implants with different pore sizes. J Mech Behav Biomed Mater.2018;84:1-11. [14] BARTOLOMEU F, COSTA MM, GOMES JR, et al. Implant surface design for improved implant stability-A study on Ti6Al4V dense and cellular structures produced by Selective Laser Melting. Tribol Int. 2019; 129:272-282. [15] POPOOLA API, PHUME L, AIGBODION VS. Laser ternary Hf-Nb-Zr composites coatings on Ti6Al4V alloy for biomedical application. Pro Inst Mech Eng Part C. 2018;233(3):1099-1107. [16] ASRI RIM, Harun WSW, Samykano M, et al. Corrosion and surface modification on biocompatible metals: A review. Mater Sci Eng C. 2017;77:1261-1274. [17] KURUP A, DHATRAK P, KHASNIS N. Surface modification techniques of titanium and titanium alloys for biomedical dental applications: A review. Mater Today Proc. 2020. doi.org/10.1016/j.matpr.2020.06.163 [18] HATAMLEH MM, WU XH, ALNAZZAWI A, et al. Surface characteristics and biocompatibility of cranioplasty titanium implants following different surface treatments. Dent Mater. 2018;34(4):676-683. [19] ZHANG YJ, QIN YG, QING YA, et al. TiCuN solid solution coating: Excellent wear-resistant biocompatible material to protect artificial joint. Mater Lett. 2018;227:145-148. [20] CHOUDHURY D, VRBKA M, MAMAT AB, et al. The impact of surface and geometry on coefficient of friction of artificial hip joints. J Mech Behav Biomed Mater. 2017;72:192-199. [21] GHOSH S, ABANTERIBA S. Status of surface modification techniques for artificial hip implants. Sci Technol Adv Mater. 2016;17(1):715-735. [22] YARIMITSU S, SASAKI S, MURAKAMI T, et al. Evaluation of lubrication properties of hydrogel artificial cartilage materials for joint prosthesis. Biosurf Biotribol. 2016;2(1):40-47. [23] GHOSH S, CHOUDHURY D, PINGGUANMURPHY B. Lubricating ability of albumin and globulin on artificial joint implants: a tribological perspective. Int J Surf Sci Eng. 2016;10(2):193. [24] ETSION I. State of the Art in Laser Surface Texturing. Adv Tribol. 2010; 761-762. [25] TIAINEN L, ABREU P, BUCIUMEANU M, et al. Novel laser surface texturing for improved primary stability of titanium implants. J Mech Behav Biomed Mater. 2019;98:26-39. [26] SAWANO H, WARISAWA S, ISHIHARA S. Study on long life of artificial joints by investigating optimal sliding surface geometry for improvement in wear resistance. Precis Eng. 2009;33(4):492-498. [27] XU Y, LI ZP, ZHANG GQ, et al. Electrochemical corrosion and anisotropic tribological properties of bioinspired hierarchical morphologies on Ti-6Al-4V fabricated by laser texturing. Tribol Int. 2019;134:352-364. [28] XU Y, LIU W, ZHANG GQ, et al. Friction stability and cellular behaviors on laser textured Ti-6Al-4V alloy implants with bioinspired micro-overlapping structures. J Mech Behav Biomed Mater. 2020;109: 103823. [29] AHUIR-TORRES JI, ARENAS MA, PERRIE W, et al. Surface texturing of aluminium alloy AA2024-T3 by picosecond laser: Effect on wettability and corrosion properties. Surf Coat Technol. 2017;321:279-291. [30] ARENAS MA, AHUIR-TORRES JI, GARCíA I, et al. Tribological behaviour of laser textured Ti6Al4V alloy coated with MoS2 and graphene. Tribol Int. 2018;128:240-247. [31] COBLAS DG, FATU A, MAOUI A, et al. Manufacturing textured surfaces: State of art and recent developments. Proc Inst Mech Eng Part J. 2014; 229(1):3-29. [32] ROY T, CHOUDHURY D, GHOSH S, et al. Improved friction and wear performance of micro dimpled ceramic-on-ceramic interface for hip joint arthroplasty. Ceram Int. 2015;41(1):681-690. [33] CHYR A, QIU MF, SPELTZ J, et al. A patterned microtexture to reduce friction and increase longevity of prosthetic hip joints. Wear. 2014; 315(1-2):51-57. [34] CHOUDHURY D, WALKER R, ROY T, et al. Performance of honed surface profiles to artificial hip joints: An experimental investigation. Int J Precis Eng Manufact. 2013;14(10):1847-1853. [35] JAVIER GF, PLANELL JA, PADRóS A, et al. The effect of shot blasting and heat treatment on the fatigue behavior of titanium for dental implant applications. Dent Mater. 2007;23(4):486-491. [36] HAVLIKOVA J, STRASKY J, VANDROVCOVA M, et al. Innovative surface modification of Ti-6Al-4V alloy with a positive effect on osteoblast proliferation and fatigue performance. Mater Sci Eng C. 2014;39:371-379. [37] HE DQ, ZHENG SX, PU JB, et al. Improving tribological properties of titanium alloys by combining laser surface texturing and diamond-like carbon film. Tribol Int. 2015;82:20-27. [38] ITO H, KANEDA K, YUHTA T, et al. Reduction of polyethylene wear by concave dimples on the frictional surface in artificial hip joints. J Arthroplasty. 2000;15(3):332-338. [39] LI KM, WANG YF, YU Z, et al. Process mechanism in laser peen texturing artificial joint material. Opt Lasers Eng. 2019;115:149-160. [40] RAMSKOGLER C, WARCHOMICKA F, MOSTOFI S, et al. Innovative surface modification of Ti6Al4V alloy by electron beam technique for biomedical application. Mater Sci Eng C. 2017;78:105-113. [41] CHOUDHURY D, URBAN F, VRBKA M, et al. A novel tribological study on DLC-coated micro-dimpled orthopedics implant interface. J Mech Behav Biomed Mater. 2015;45:121-131. [42] CHING HA, CHOUDHURY D, NINE MJ, et al. Effects of surface coating on reducing friction and wear of orthopaedic implants. Sci Technol Adv Mater. 2016;15(1):506-512. [43] JIN XD, YANG XK, WEI FR, et al. Research progress of surface modification materials and technology for medical titanium and titanium alloys. World Nonferrous Met. 2018;(7):265-266,268. [44] NGUYEN-TRI P, NGUYEN TA, CARRIERE P, et al. Nanocomposite Coatings: Preparation, Characterization, Properties, and Applications. Int J Corros. 2018;2018:4749501.1-4749501.19. [45] EGE D, DURU L, KAMALI AR, et al. Nitride, Zirconia, Alumina, and Carbide Coatings on Ti6Al4V Femoral Heads: Effect of Deposition Techniques on Mechanical and Tribological Properties. Adv Eng Mater. 2017;19(11):49-54. [46] SONNTAG R, REINDERS J, KRETZER JP. What’s next? Alternative materials for articulation in total joint replacement. Acta Biomater. 2012;8(7):2434-2441. [47] ŁAPAJ Ł, WENDLAND J, MARKUSZEWSKI J, et al. Retrieval analysis of titanium nitride (TiN) coated prosthetic femoral heads articulating with polyethylene. J Mech Behav Biomed Mater. 2015;55:127-139. [48] ZUO J, XIE YN, ZHANG J, et al. TiN coated stainless steel bracket: Tribological, corrosion resistance, biocompatibility and mechanical performance. Surf Coat Technol. 2015;277:227-233. [49] MARIN E, OFFOIACH R, LANZUTTI A, et al. Hybrid diffusive/PVD treatments to improve the tribological resistance of Ti-6Al-4V. Bio Med Mater Eng. 2013;23:601-612. [50] ZHANG X, SUN S, SU D, et al. Structure and properties of TiCuN coatings by HCD assisted AIP. Surf Eng. 2016;32(3):223-228. [51] MULLIGAN CP, GALL D. CrN–Ag self-lubricating hard coatings. Surf Coat Technol. 2005;200(5):1495-1500. [52] KSTENBAUER H, FONTALVO GA, MITTERER C, et al. Tribological Properties of TiN/Ag Nanocomposite Coatings. Tribol Lett. 2008;30(1):53-60. [53] LIU C, BI Q, MATTHEWS A. Tribological and electrochemical performance of PVD TiN coatings on the femoral head of Ti–6Al–4V artificial hip joints. Surf Coat Technol. 2003;163:597-604. [54] BALLARRE J, MANJUBALA I, SCHREINER WH, et al. Improving the osteointegration and bone–implant interface by incorporation of bioactive particles in sol–gel coatings of stainless steel implants. Acta Biomater. 2010;6(4):1601-1609. [55] TARNOWSKI M, KULIKOWSKI K, BOROWSKI T, et al. Influence of amorphous carbon layers on tribological properties of polyetheretherketone composite in contact with nitrided layer produced on Ti6Al4V titanium alloy. Diamond Relat Mater. 2017; 75:123-130. [56] XIE D, LIU HJ, DENG XR, et al. Deposition of a-C:H films on UHMWPE substrate and its wear-resistance. Appl Surf Sci. 2009; 256(1):284-288. [57] ŻóRAWSKI W, CHATYS R, RADEK N, et al. Plasma-sprayed composite coatings with reduced friction coefficient. Surf Coat Technol. 2008; 202(18):4578-4582. [58] BALANI K, CHEN Y, HARIMKAR SP, et al. Tribological behavior of plasma-sprayed carbon nanotube-reinforced hydroxyapatite coating in physiological solution. Acta Biomater. 2007;3(6):944-951. [59] DONG ZL, KHOR KA, QUEK CH, et al. TEM and STEM analysis on heat-treated and in vitro plasma-sprayed hydroxyapatite/Ti-6Al-4V composite coatings. Biomaterials. 2003;24(1):97-105. [60] LIANG H, SHI B, FAIRCHILD A, et al. Applications of plasma coatings in artificial joints: an overview. Vacuum. 2004;73(3-4):317-326. [61] JIN J, CHEN YB, GAO KW, et al. The effect of ion implantation on tribology and hot rolling contact fatigue of Cr4Mo4Ni4V bearing steel. Appl Surf Sci. 2014;305:93-100. [62] ZHOU ZF, LI KY, SHUM P, et al. Surface gradient CoCrMo alloy generated by carbon ion implantation with enhanced tribocorrosion resistance. Surf Coat Technol. 2017;320:590-594. [63] PARK WW, KIM EK, JEON JH, et al. Wear of UHMWPE against nitrogen-ion-implanted and NbN-coated Co–Cr–Mo alloy formed by plasma immersion ion implantation and deposition for artificial joints. Appl Surf Sci. 2012;258(20):8228-8233. [64] NAVINSEK B, SEAL S. Transition metal nitride functional coatings. JOM. 2001;53(9):51-54. [65] COADOU CL, KARST N, EMIEUX F, et al. Assessment of ultrathin yttria-stabilized zirconia foils for biomedical applications. J Mater Sci. 2017; 50(18):1-11. [66] SONG J, LIU YH, LIAO ZH, et al. Wear studies on ZrO2-filled PEEK as coating bearing materials for artificial cervical discs of Ti6Al4V. Mater Sci Eng C Mater Biol Appl. 2016;69:985-994. [67] MCCALDEN RW, CHARRON KD, DAVIDSON RD, et al. Damage of an Oxinium femoral head and polyethylene liner following ‘routine’ total hip replacement. J Bone Jt Surg Br Vol. 2011;93(3):409. [68] SUNDARARAJAN G, KRISHNA LR. Mechanisms underlying the formation of thick alumina coatings through the MAO coating technology. Surf Coat Technol. 2003;167(2-3):269-277. |
| [1] | Bi Jintong, Hu Xin, Liu Jinshu. Wear properties of dental ceramics [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 406-412. |
| [2] | Jin Tao, Liu Lin, Zhu Xiaoyan, Shi Yucong, Niu Jianxiong, Zhang Tongtong, Wu Shujin, Yang Qingshan. Osteoarthritis and mitochondrial abnormalities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1452-1458. |
| [3] | Zhang Lichuang, Xu Hao, Ma Yinghui, Xiong Mengting, Han Haihui, Bao Jiamin, Zhai Weitao, Liang Qianqian. Mechanism and prospects of regulating lymphatic reflux function in the treatment of rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1459-1466. |
| [4] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhou Qian, Zhang Qiang, Chen Qiu. Human salivary components and osteoporosis/osteopenia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1439-1444. |
| [5] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [6] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhang Qiang, Liu Jing, Shao Ming. Acupuncture for Parkinson’s disease: an insight into the action mechanism in animal experiments [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1272-1277. |
| [7] | Guo Jia, Ding Qionghua, Liu Ze, Lü Siyi, Zhou Quancheng, Gao Yuhua, Bai Chunyu. Biological characteristics and immunoregulation of exosomes derived from mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1093-1101. |
| [8] | Wu Weiyue, Guo Xiaodong, Bao Chongyun. Application of engineered exosomes in bone repair and regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1102-1106. |
| [9] | Zhou Hongqin, Wu Dandan, Yang Kun, Liu Qi. Exosomes that deliver specific miRNAs can regulate osteogenesis and promote angiogenesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1107-1112. |
| [10] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [11] | Huang Chenwei, Fei Yankang, Zhu Mengmei, Li Penghao, Yu Bing. Important role of glutathione in stemness and regulation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1119-1124. |
| [12] | Hui Xiaoshan, Bai Jing, Zhou Siyuan, Wang Jie, Zhang Jinsheng, He Qingyong, Meng Peipei. Theoretical mechanism of traditional Chinese medicine theory on stem cell induced differentiation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1125-1129. |
| [13] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [14] | Fan Yiming, Liu Fangyu, Zhang Hongyu, Li Shuai, Wang Yansong. Serial questions about endogenous neural stem cell response in the ependymal zone after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1137-1142. |
| [15] | Xu Lei, Han Xiaoqiang, Zhang Jintao, Sun Haibiao. Hyaluronic acid around articular chondrocytes: production, transformation and function characteristics [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 768-773. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||