Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (27): 4354-4360.doi: 10.12307/2021.196
Previous Articles Next Articles
Fixation of the modified Pauwels type Ⅲ femoral neck fractures in young adults with percutaneous hollow compression screw combined with medial buttress plate: 2-year follow-up
Ren Sijun, Cao Zhipeng, Xu Rao, Ru Jiangying
- Affiliated Hospital of Yangzhou University, Yangzhou 225000, Jiangsu Province, China
-
Received:2020-11-28Revised:2020-12-04Accepted:2020-12-31Online:2021-09-28Published:2021-04-10 -
Contact:Ru Jiangying, MD, Chief physician, Associate professor, Master’s supervisor, Affiliated Hospital of Yangzhou University, Yangzhou 225000, Jiangsu Province, China -
About author:Ren Sijun, Master candidate, Affiliated Hospital of Yangzhou University, Yangzhou 225000, Jiangsu Province, China -
Supported by:the Scientific Research Project of Jiangsu Provincial Health and Family Planning Commission, No. H201662 (to RJY); the Key Research and Development (Social Development) Funding Project of Yangzhou City, No. YZ2018086 (to RJY)
CLC Number:
Cite this article
Ren Sijun, Cao Zhipeng, Xu Rao, Ru Jiangying. Fixation of the modified Pauwels type Ⅲ femoral neck fractures in young adults with percutaneous hollow compression screw combined with medial buttress plate: 2-year follow-up[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4354-4360.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
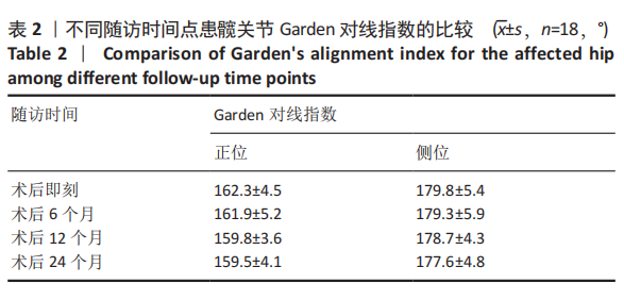
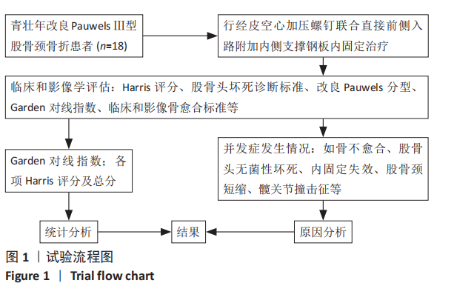
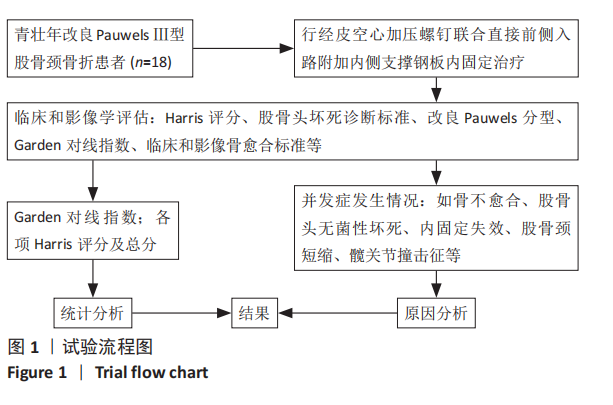
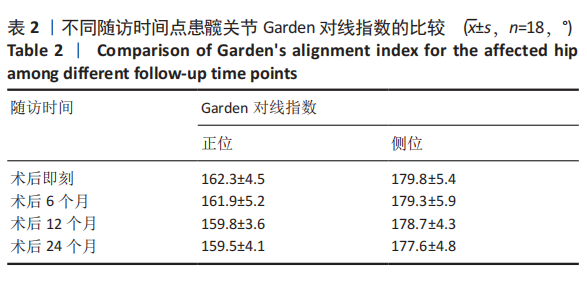
2.3 一般情况 18例患者受伤至入院时间2-52 h,平均(8.8±5.7) h;受伤到手术时间24-112 h,平均(46.6±6.3) h;手术时间62-128 min,平均(88.6±11.4) min;平均术后部分负重时间及完全负重时间分别为(3.1±0.6)个月(2.5-4.3个月)和(5.5±0.7)个月(4.6-7.2个月);平均影像骨愈合时间和临床骨愈合时间分别为(4.3±1.1)个月(3.8-6.1个月)和(5.8±0.9)个月(4.9-8.2个月)。 2.4 影像学评估结果 采用Garden对线指数评估不同时间点的股骨颈复位质量,术后6,12,24个月的患髋关节Garden对线指数与术后即刻相比,差异均无显著性意义(P > 0.05),见表2。"
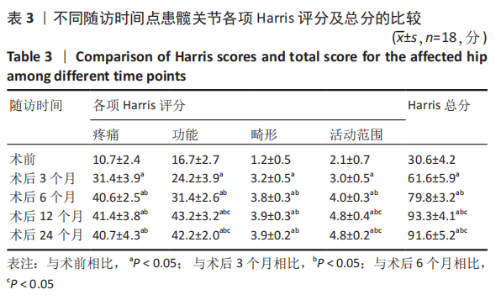
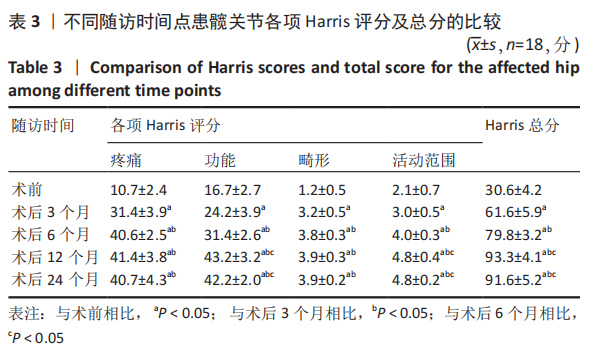
2.5 疗效评价 通过不同时间点的患髋Harris评分评价术后髋关节功能恢复情况。结果显示,术后3,6,12,24个月,患髋的各项Harris评分及总分均显著高于术前,差异有显著性意义(P < 0.05);术后6,12,24个月,患髋的各项Harris评分及总分与术后3个月相比均显著改善,差异有显著性意义(P < 0.05);与术后6个月相比,术后12,24个月患髋功能、活动范围及总分均显著改善,差异有显著性意义(P < 0.05);但在疼痛、畸形方面,术后6,12,24个月两两比较差异均无显著性意义(P > 0.05);术后12,24个月,患髋的各项Harris评分及总分,两两比较差异均无显著性意义(P > 0.05),见表3。"
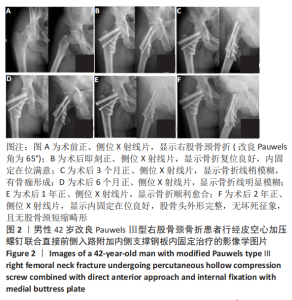
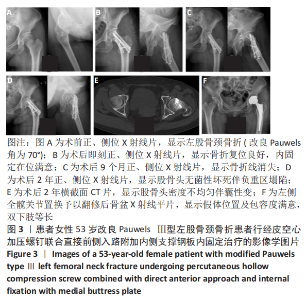
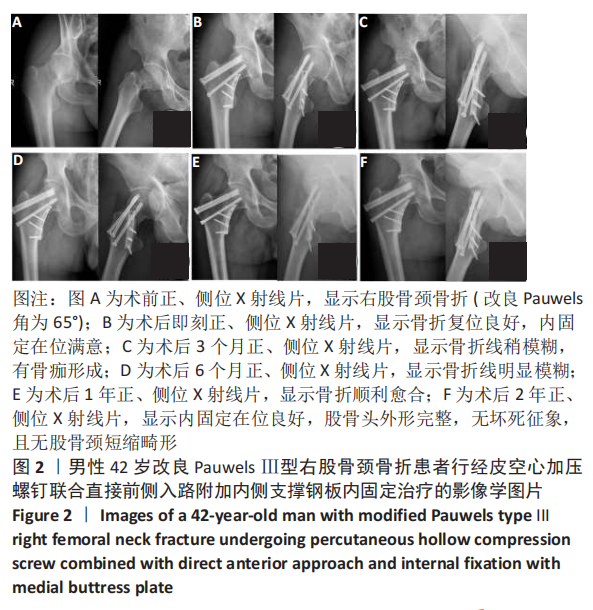
2.6 并发症发生情况 此组18例患者中,2例患者术后发生空心加压螺钉退出伴股骨颈短缩(约8 mm),但最终顺利完成临床骨愈合;1例患者术后2年随访时发生股骨头无菌性坏死塌陷,伴有患髋关节功能障碍,随后行直接前侧入路人工全髋关节置换予以翻修;1例患者髋关节过度屈曲时出现明显疼痛,考虑与内侧支撑钢板过长和髋臼前下缘撞击有关,术后3个月症状缓解。所有患者伤口一级愈合,均无骨折不愈合、下肢深静脉血栓、坠积性肺炎及压疮等并发症发生。 2.7 材料与宿主生物相容性 所有患者均未出现与植入物材料相关的不良事件,植入物生物相容性良好。 2.8 典型病例 典型病例1:患者男性,42岁,高处坠落致右股骨颈骨折(改良Pauwels Ⅲ型),既往体健,无其他基础疾病,行经皮空心加压螺钉联合直接前侧入路附加MBP内固定治疗,见图2。"
| [1] SLOBOGEAN GP, SPRAGUE SA, SCOTT T, et al. Complications following young femoral neck fractures. Injury. 2015;46(3):484-491. [2] LY TV, SWIONTKOWSKI MF. Treatment of Femoral Neck Fractures in Young Adults. J Bone Joint Surg Am. 2008;90A(10):2254-2266. [3] UPADHYAY A, JAIN P, MISHRA P, et al. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86(7):1035-1040. [4] DAVIDOVITCH RI, JORDAN CJ, EGOL KA, et al. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236-242. [5] MIR H, COLLINGE C. Application of a medial buttress plate may prevent many treatment failures seen after fixation of vertical femoral neck fractures in young adults. Med Hypotheses. 2015;84(5):429-433. [6] 李文龙, 梅沉成, 范亚楠, 等. 1/3管状板联合空心加压螺钉内固定术治疗青壮年 Pauwels Ⅱ、Ⅲ型股骨颈骨折43例[J]. 山东医药, 2016,56(27):92-94. [7] PUTNAM SM, COLLINGE CA, GARDNER MJ, et al. Vascular Anatomy of the Medial Femoral Neck and Implications for Surface Plate Fixation. J Orthop Trauma. 2019;33(3):111-115. [8] STACEY SC, RENNINGER CH, HAK D, et al. Tips and tricks for ORIF of displaced femoral neck fractures in the young adult patient. Eur J Orthop Surg Traumatol. 2016;26(4):355-363. [9] WANG S, YANG J, SHEN H, et al. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury. 2015;46(10):1969-1974. [10] GARDEN RS. Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br. 1971;53(2):183-197. [11] MOLNAR RB, ROUTT MJ. Open reduction of intracapsular hip fractures using a modified Smith-Petersen surgical exposure. J Orthop Trauma. 2007;21(7):490-494. [12] LUTTRELL K, BELTRAN M, COLLINGE CA. Preoperative decision making in the treatment of high-angle “vertical” femoral neck fractures in young adult patients. An expert opinion survey of the Orthopaedic Trauma Association’s (OTA) membership. J Orthop Trauma. 2014;28(9): e221-e225. [13] STANNARD JP, HARRIS HW, VOLGAS DA, et al. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;(377):44-56. [14] YE Y, HAO J, MAUFFREY C, et al. Optimizing Stability in Femoral Neck Fracture Fixation. Orthopedics. 2015;38(10):625-630. [15] 杨义,于志亮,郭连霞,等.同种异体腓骨段联合加压空心钉内固定术治疗青壮年股骨颈移位骨折[J]. 中国医师杂志,2014(z1):119-120. [16] KUNAPULI SC, SCHRAMSKI MJ, LEE AS, et al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma. 2015;29(3):144-150. [17] GUMUSTAS SA, TOSUN HB, AGIR I, et al. Influence of number and orientation of screws on stability in the internal fixation of unstable femoral neck fractures. Acta Orthop Traumatol Turc. 2014;48(6):673-678. [18] GIORDANO V, ALVES DD, PAES RP, et al. The role of the medial plate for Pauwels type III femoral neck fracture: a comparative mechanical study using two fixations with cannulated screws. J Exp Orthop. 2019;6(1):18. [19] 周孝乾, 田智勇, 陈洪强, 等. 比基尼入路切开复位PFNA与闭合空心钉治疗青壮年股骨颈骨折的疗效比较[J]. 中华老年骨科与康复电子杂志,2020,6(5):251-256. [20] 杨晓秋, 赵滨, 叶赟, 等. 切开复位PFNA内固定治疗青壮年移位型股骨颈骨折近期疗效观察[J]. 贵州医药,2018,42(8):998-999. [21] ZLOWODZKI M, AYENI O, PETRISOR BA, et al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163-169. [22] 丁强, 孙楠, 吴非燃, 等. 空心钉附加内侧支撑钢板内固定治疗青壮年非头下型股骨颈骨折的疗效观察[J]. 中国骨与关节损伤杂志, 2018,33(5):534-535. [23] YE Y, CHEN K, TIAN K, et al. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury. 2017;48(10):2189-2193. [24] ZHUANG L, WANG L, XU D, et al. Anteromedial femoral neck plate with cannulated screws for the treatment of irreducible displaced femoral neck fracture in young patients: a preliminary study. Eur J Trauma Emerg Surg. 2019;45(6):995-1002. [25] 林绪超, 何文, 郑竑, 等. 经皮空心钉联合DAA入路微创支撑钢板内固定治疗青壮年Pauwels Ⅲ型股骨颈骨折的近期疗效[J]. 中国骨与关节损伤杂志,2019,34(6):593-595. [26] MARCHAND LS, KARNS M, HIGGINS TF, et al. Femoral Neck Fracture Fixation with a Medial Buttress Plate That Led to Impingement with Hip Flexion: A Case Report. JBJS Case Connect. 2019;9(1):e21. [27] ZLOWODZKI M, AYENI O, PETRISOR BA, et al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163-169. [28] GAUTIER E, GANZ K, KRUGEL N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679-683. [29] LAZARO LE, KLINGER CE, SCULCO PK, et al. The terminal branches of the medial femoral circumflex artery: the arterial supply of the femoral head. Bone Joint J. 2015;97-B(9):1204-1213. [30] PAPAKOSTIDIS C, PANAGIOTOPOULOS A, PICCIOLI A, et al. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome.Injury. 2015;46(3):459-466. [31] SLOBOGEAN GP, SPRAGUE SA, SCOTT T, et al. Management of young femoral neck fractures: is there a consensus? Injury. 2015;46(3):435-440. |
| [1] | Xu Xinzhong, Wu Zhonghan, Yu Shuisheng, Zhao Yao, Xu Chungui, Zhang Xin, Zheng Meige, Jing Juehua. Biomechanical analysis of different ways of inserting Steinmann Pins into the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1313-1317. |
| [2] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [3] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [4] | Zheng Yongze, Zheng Liqin, He Xingpeng, Chen Xinmin, Li Musheng, Li Pengfei, Lin Ziling. Extended finite element modeling analysis of femoral neck fracture based on ABAQUS software [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 853-857. |
| [5] | Liang Haoran, Zhou Xin, Yang Yanfei, Niu Wenjie, Song Wenjie, Ren Zhiyuan, Wang Xueding, Liu Yang, Duan Wangping. Pathogenesis of femoral head necrosis after internal fixation of femoral neck fractures in young adults [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 456-460. |
| [6] | Wang Chong, Zhang Meiying, Zhou Jian, Lao Kecheng. Early gait changes after total hip arthroplasty through direct anterior approach and posterolateral approach [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 359-364. |
| [7] | Hu Junxian, Zhao Deying, Wang Lei, Huang Minghuo, Wu Yalan, Chen Jincao, Liu Zheng. Complication comparison and application improvement of 3D-printed plastic polyetherketone and titanium mesh cranioplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3327-3331. |
| [8] | Yan Kun, Mou Limin, Yang Xiaohui, Wang Jian, Ran Jian. Finite element analysis of Pauwels type III femoral neck fracture fixed with three configurations of cannulated screws [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2807-2811. |
| [9] | Wang Lei, Li Jia, Li Tao, Liu Limin, Suonan Angxiu. Femoral neck system for internal fixation of femoral neck fracture in high altitude areas [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2844-2848. |
| [10] | Liu Chen, Hu Chengzhe, Yin Xun, Yu Ziheng, Yang Jiandong. Risk factors of residual pain after percutaneous vertebral augmentation for osteoporotic thoracolumbar compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2900-2905. |
| [11] | Zhao Haifeng, Dai Yiping, Zhu Wenyu, Yan Ke, Wang Yu, Wu Jie, Gu Donghua, Xu Xiaofeng, Cao Longxing, Huang Qiang. Reasons for failure of silica gel and titanium mesh in cranioplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2522-2525. |
| [12] | Wang Jiaqi, Luo Xiaozhong, Tong Yi, Shi Weixiang, Ding Yong, Zhou Xin, Wu Gang. Pauwels type III femoral neck fracture treated with three and four cannulated screws assisted by robot navigation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(15): 2352-2355. |
| [13] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [14] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [15] | Wang Sizhe, Gao Haiyan, Lan Xiaoquan, Wang Pan, Huang Haoran, Wang Jinyu, Ma Jianlin. A short-term evaluation of three-dimensional printed guide plate assisted hollow screw in the treatment of non-displaced femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5753-5758. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||