[1] TSANG B, STOTHERS L, MACNAB A, et al. A systematic review and comparison of questionnaires in the management of spinal cord injury, multiple sclerosis and the neurogenic bladder. Neurourol Urodyn. 2016;35(3):354-364.
[2] ZHANG T, LIU H, LIU Z, et al. Acupuncture for neurogenic bladder due to spinal cord injury: a systematic review protocol. BMJ Open. 2014;4(9):e006249 .
[3] LOY K, BAREYRE FM. Rehabilitation following spinal cord injury: how animal models can help our understanding of exercise-induced neuroplasticity. Neural Regen Res. 2019;14(3):405-412.
[4] 闫鹏.新型骶神经根刺激器在脊髓损伤后神经源性膀胱功能重建中的初步应用[D].长春:吉林大学,2011.
[5] 王潇然.长期骶神经前根阳极阴滞电刺激对兔完全脊髓损伤性神经源性膀胱功能恢复的作用[D].长春:吉林大学,2011.
[6] The Ministry of Science and Technology of the People’s Republic of China. Guidance Suggestions (Instructions) for the Care and Use of Laboratory Animals. 2006-09-30.
[7] 王春昕,潘肃,张善勇,等.长期阳极阻滞电刺激对脊髓损伤后膀胱功能重建作用研究[J].中国实验诊断学,2017,21(8):1438-1441.
[8] 闫鹏,郑伟东,谭云冰,等.电刺激脊髓损伤模型兔肛周皮肤调控神经源性膀胱内压[J].中国组织工程研究,2015,19(49):7932-7937.
[9] YAN P, YANG YX, GAO Q, et al. Electrical stimulation of the sacral nerve anterior root following induced bladder detrusor contraction. Neural Regen Res. 2010;5(24):1900-1904.
[10] DOYLE C, CRISTOFARO V, SACK BS, et al. The role of the mucosa in modulation of evoked responses in the spinal cord injured rat bladder. Neurourol Urodyn. 2018;37(5):1583 -1593.
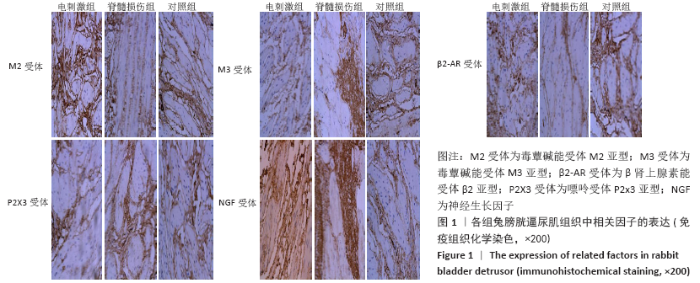
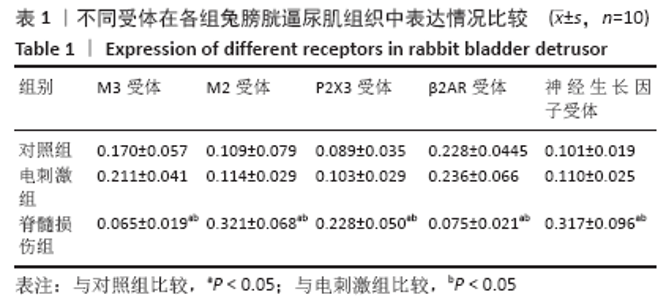
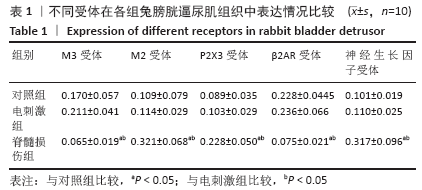
[11] SCHULTE-BAUKLOH H, PRIEFERT J, knispel HH, et al. Botulinum toxin A detrusor injections reduce postsynaptic muscular M2, M3, P2X2, and P2X3 receptors in children and adolescents who have neurogenic detrusor overactivity: a single-blind study. Urology. 2013;81(5): 1052-1057.
[12] CHANDRASEKARAN S, DAVIS J, BERSCH I, et al. Electrical stimulation and denervated muscles after spinal cord injury. Neural Regen Res. 2020;15(8):1397-1407.
[13] OQODA M, FUCHIHATA Y, ONOUE S, et al. Characterization of muscarinic and P2X receptors in the urothelium and detrusor muscle of the rat bladder. J Pharmacol Sci. 2016;131(1):58-63.
[14] MUNOZ A, SOMOGYI GT, BOONE TB, et al. Modulation of bladder afferent signals in normal and spinal cord-injured rats by purinergic P2X3 and P2X2/3 receptors. BJU Int. 2012;110(8):E409-E414.
[15] COELHO A, ANTUNES-LOPES T, GILLESPIE J, et al. Beta-3 adrenergic receptor is expressed in acetylcholine-containing nerve fibers of the human urinary bladder: an immunohistochemical study. Neurourol urodyn. 2017;36(8):1972-1980.
[16] 曹文峰.β3-AR调节逼尿肌舒张功能的作用及信号分子机制的实验研究[D].重庆:第三军医大学,2003.
[17] EDMONDSON SD, ZHU C, KAR NF, et al. Discovery of vibegron: a potent and selective β3 adrenergic receptor agonist for the treatment of overactive bladder. J Med Chem. 2016;59(2):609-623.
[18] MICHEL MC, SAND C. Effect of pre-contraction on β-adrenoceptor-mediated relaxation of rat urinary bladder. World J Urol. 2009;27(6): 711-715.
[19] KASHYAP M, PORE S, YOSHIMURA N, et al. Constitutive expression Of NGF And P75(NTR) affected by bladder distension and NGF antisense treatment. Life Sci. 2016;148:93-98.
[20] Naoki W, Takahiro S, Nobutaka S, et al. The effect of neutralization of nerve growth factor (NGF) on bladder and urethral dysfunction in mice with spinal cord injury. Neurourol urodyn. 2018;37(6):1889-1896.
|