[1] CLYNES MA, HARVEY NC, CURTIS EM, et al. The epidemiology of osteoporosis. Br Med Bull. 2020;133(1):105-117.
[2] YOSHIDA S, IKEDO A, YANAGIHARA Y, et al. Bub1 suppresses inflammatory arthritis-associated bone loss in mice through inhibition of TNFα-mediated osteoclastogenesis. J Bone Miner Res. 2024;39(3):341-356.
[3] CLÉZARDIN P, COLEMAN R, PUPPO M, et al. Bone metastasis: mechanisms, therapies, and biomarkers. Physiol Rev. 2021;101(3):797-855.
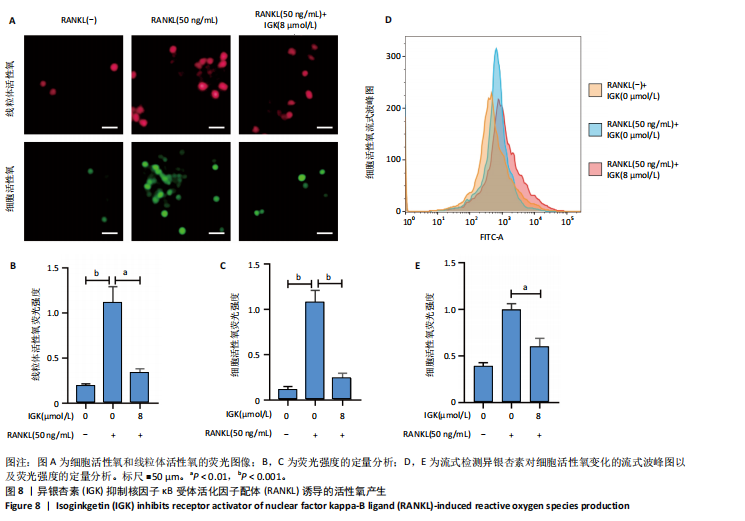
[4] LI H, DENG W, YANG J, et al. Corylifol A suppresses osteoclastogenesis and alleviates ovariectomy-induced bone loss via attenuating ROS production and impairing mitochondrial function. Biomed Pharmacother. 2024;171:116166.
[5] HE J, ZHENG L, LI X, et al. Obacunone targets macrophage migration inhibitory factor (MIF) to impede osteoclastogenesis and alleviate ovariectomy-induced bone loss. J Adv Res. 2023;53:235-248.
[6] HÄNDEL MN, CARDOSO I, VON BÜLOW C, et al. Fracture risk reduction and safety by osteoporosis treatment compared with placebo or active comparator in postmenopausal women: systematic review, network meta-analysis, and meta-regression analysis of randomised clinical trials. BMJ. 2023;381:e068033.
[7] GU Q, YANG H, SHI Q. Macrophages and bone inflammation. J Orthop Translat. 2017;10:86-93.
[8] LI H, DENG W, QIN Q, et al. Isoimperatorin attenuates bone loss by inhibiting the binding of RANKL to RANK. Biochem Pharmacol. 2023; 211:115502.
[9] FANG C, GUO JW, WANG YJ, et al. Diterbutyl phthalate attenuates osteoarthritis in ACLT mice via suppressing ERK/c-fos/NFATc1 pathway, and subsequently inhibiting subchondral osteoclast fusion. Acta Pharmacol Sin. 2022;43(5):1299-1310.
[10] CHEN X, ZHI X, WANG J, et al. RANKL signaling in bone marrow mesenchymal stem cells negatively regulates osteoblastic bone formation. Bone Res. 2022;10(1):54.
[11] LI Y, ZHUANG Q, TAO L, et al. Urolithin B suppressed osteoclast activation and reduced bone loss of osteoporosis via inhibiting ERK/NF-κB pathway. Cell Prolif. 2022;55(10):e13291.
[12] XU H, JIA Y, LI J, et al. Niloticin inhibits osteoclastogenesis by blocking RANKL-RANK interaction and suppressing the AKT, MAPK, and NF-κB signaling pathways. Biomed Pharmacother. 2022;149:112902.
[13] YUE H, TIAN Y, LI Y, et al. Comparative study of holothurin A and echinoside A on inhibiting the high bone turnover via downregulating PI3K/AKT/β-catenin and OPG/RANKL/NF-κB signaling in ovariectomized mice. Food Funct. 2022;13(8):4748-4756.
[14] MOON JB, KIM JH, KIM K, et al. Akt induces osteoclast differentiation through regulating the GSK3β/NFATc1 signaling cascade. J Immunol. 2012;188(1):163-169.
[15] WU X, HUANG J, TANG J, et al. Isoginkgetin, a bioactive constituent from Ginkgo Biloba, protects against obesity-induced cardiomyopathy via enhancing Nrf2/ARE signaling. Redox Biol. 2022;57:102485.
[16] KESTI S, MACAR O, KALEFETOĞLU MACAR T, et al. Investigation of the protective role of Ginkgo biloba L. against phytotoxicity, genotoxicity and oxidative damage induced by Trifloxystrobin. Sci Rep. 2024;14(1):19937.
[17] WANG R, SHAO X, YANG J, et al. Ginkgo biloba Extract Mechanism Inhibits Hepatocellular Carcinoma through the Nuclear Factor-κB/p53 Signaling Pathway. J Environ Pathol Toxicol Oncol. 2020;39(2):179-189.
[18] CAO F, QIN KR, KANG K, et al. Ginkgo biloba L. extract prevents steroid-induced necrosis of the femoral head by rescuing apoptosis and dysfunction in vascular endothelial cells via the PI3K/AKT/eNOS pathway. J Ethnopharmacol. 2022;296:115476.
[19] WANG A, YANG Q, LI Q, et al. Ginkgo Biloba L. Extract Reduces H2O2-Induced Bone Marrow Mesenchymal Stem Cells Cytotoxicity by Regulating Mitogen-Activated Protein Kinase (MAPK) Signaling Pathways and Oxidative Stress. Med Sci Monit. 2018;24:3159-3167.
[20] DENG W, DING Z, WANG Y, et al. Dendrobine attenuates osteoclast differentiation through modulating ROS/NFATc1/MMP9 pathway and prevents inflammatory bone destruction. Phytomedicine. 2022; 96:153838.
[21] AN Y, ZHANG H, WANG C, et al. Activation of ROS/MAPKs/NF-κB/NLRP3 and inhibition of efferocytosis in osteoclast-mediated diabetic osteoporosis. FASEB J. 2019;33(11):12515-12527.
[22] CHENG C, WENTWORTH K, SHOBACK DM. New Frontiers in Osteoporosis Therapy. Annu Rev Med. 2020;71:277-288.
[23] LEBOFF MS, GREENSPAN SL, INSOGNA KL, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022;33(10):2049-2102.
[24] KHANDELWAL S, LANE NE. Osteoporosis: Review of Etiology, Mechanisms, and Approach to Management in the Aging Population. Endocrinol Metab Clin North Am. 2023;52(2):259-275.
[25] YU B, WANG CY. Osteoporosis and periodontal diseases - An update on their association and mechanistic links. Periodontol 2000. 2022; 89(1):99-113.
[26] WEI L, CHEN W, HUANG L, et al. Alpinetin ameliorates bone loss in LPS-induced inflammation osteolysis via ROS mediated P38/PI3K signaling pathway. Pharmacol Res. 2022;184:106400.
[27] HU M, YAN H, LI H, et al. Use of network pharmacology and molecular docking to explore the mechanism of action of curcuma in the treatment of osteosarcoma. Sci Rep. 2023;13(1):9569.
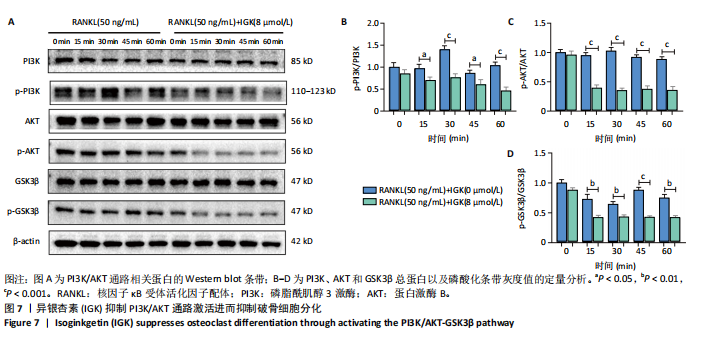
[28] LU J, SHI X, FU Q, et al. New mechanistic understanding of osteoclast differentiation and bone resorption mediated by P2X7 receptors and PI3K-Akt-GSK3β signaling. Cell Mol Biol Lett. 2024;29(1):100.
[29] WANG L, SHI X, ZHAO R, et al. Calcitonin-gene-related peptide stimulates stromal cell osteogenic differentiation and inhibits RANKL induced NF-kappaB activation, osteoclastogenesis and bone resorption. Bone. 2010;46(5):1369-1379.
[30] CHEN ZH, WU JJ, GUO DY, et al. Physiological functions of podosomes: From structure and function to therapy implications in osteoclast biology of bone resorption. Ageing Res Rev. 2023;85:101842.
[31] ZENG XZ, HE LG, WANG S, et al. Aconine inhibits RANKL-induced osteoclast differentiation in RAW264.7 cells by suppressing NF-κB and NFATc1 activation and DC-STAMP expression. Acta Pharmacol Sin. 2016;37(2):255-263.
[32] WU L, LUO Z, LIU Y, et al. Aspirin inhibits RANKL-induced osteoclast differentiation in dendritic cells by suppressing NF-κB and NFATc1 activation. Stem Cell Res Ther. 2019;10(1):375.
[33] PANG M, RODRÍGUEZ-GONZALEZ M, HERNANDEZ M, et al. AP-1 and Mitf interact with NFATc1 to stimulate cathepsin K promoter activity in osteoclast precursors. J Cell Biochem. 2019;120(8):12382-12392.
[34] CHEN K, QIU P, YUAN Y, et al. Pseurotin A Inhibits Osteoclastogenesis and Prevents Ovariectomized-Induced Bone Loss by Suppressing Reactive Oxygen Species. Theranostics. 2019;9(6):1634-1650.
[35] LI J, WEI JJ, WU CH, et al. Epimedin A inhibits the PI3K/AKT/NF-κB signalling axis and osteoclast differentiation by negatively regulating TRAF6 expression. Mol Med. 2024;30(1):125.
[36] IANTOMASI T, ROMAGNOLI C, PALMINI G, et al. Oxidative Stress and Inflammation in Osteoporosis: Molecular Mechanisms Involved and the Relationship with microRNAs. Int J Mol Sci. 2023;24(4):3772.
[37] AGIDIGBI TS, KIM C. Reactive Oxygen Species in Osteoclast Differentiation and Possible Pharmaceutical Targets of ROS-Mediated Osteoclast Diseases. Int J Mol Sci. 2019;20(14):3576.
[38] PENG Q, WANG J, HAN M, et al. Tanshinone IIA inhibits osteoclastogenesis in rheumatoid arthritis via LDHC-regulated ROS generation. Chin Med. 2023;18(1):54.
[39] HUANG J, SONG D, XU M, et al. Trifolirhizin reduces osteoclast formation and prevents inflammatory osteolysis by inhibiting RANKL-induced activation of NF-kappaB and MAPK signaling pathways and ROS. Phytother Res. 2024;38(9):4650-4666.
[40] REID IR, BILLINGTON EO. Drug therapy for osteoporosis in older adults. Lancet. 2022;399(10329):1080-1092.
|