椎间融合是重建脊椎稳定性、纠正腰椎异常应力承载方式的有效方法
[15]。脊柱融合手术的稳定性于1911年被Hibbs等首次报道,椎体间融合是脊柱附合的理想方法这一理念于1936年由Mercer 首次提出。后方入路腰椎体间融合治疗下腰痛于20世纪40年代由Cloward应用于临床,并且取得良好的手术效果, Stock改良了前路椎体融合并促进该术式获得长足的发展,20世纪80年代,后方入路椎体间融合又再次被临床广泛应用,但由于植骨块的强度不足及植骨块形状的不规则而不能充分保证椎体间融合,导致融合节段的稳定性不足,术后可能发生植骨块被吸收引起的椎体间高度丢失及植骨块移位导致的神经卡压等并发症,各种单纯植骨融合术后假关节率高达30%-60%。由于植骨块的缺陷,椎间融合器被发明,首先应用于马的Wobbler综合征的治疗,被进一步改进后应用于人的下腰痛的治疗。腰椎间盘突出症经典手术同时行椎间融合的目的是恢复椎体间高度,稳定腰椎及防治椎间盘突出复发。当伴有椎体滑脱及脊柱不稳时,单纯手术减压和椎间盘摘除会进一步破坏脊柱的稳定性,而椎间融合的作用是恢复脊柱的稳定性,承载应力、保持椎间隙高度,从而使韧带和肌肉维持适当张力,达到维持椎体稳定的目的。
椎间融合是脊柱疾病中一种有效的手术方式,该手术方法能有效恢复脊柱的稳定性,但是有研究发现单节段或多节段融合可导致相邻节段的退变。Phillips等[16]通对兔腰椎融合内固定模型的研究,发现在融合后3个月时,可见融合相邻节段椎间盘的外观和结构出现紊乱,从而推论出椎间融合加重了相邻节段椎间盘的退步。Chen等[17]通过有限元模型研究腰椎前路融合术后相邻节段椎间盘的压力分布,发现在屈曲、扭转、侧曲时,相邻节段椎间盘压力增加的规律是:低位融合明显高于高位融合;多阶段融合明显高于单节段融合;而且与应力强度的增加成正相关。同时,生物力学测定发现腰椎融合术后腰椎总体活动度减小,而相邻节段的活动度占整个腰椎运动的比例增加。因此,部分作者认为,脊柱融合术会导致相邻节段的退行性改变,且随着时间的延长而加重。如果相邻节段术前已存在某些退变因素,或术后出现脊柱曲度不良,则会使相邻节段退变更加迅速[18-19]。有研究结果表明,年龄是腰椎融合后加速相邻节段退变的最重要因素之一,年龄在55岁以上的腰椎后外侧融合患者,其相邻节段退变的发生率可以达到36.7%,而年龄在55岁以下的相邻节段退变发生率仅为12%。脊柱融合前相邻节段是否存在退变因素与术后退变发生率有直接关系。但也有研究发现,在融合节段的相邻节段的上一节段也可出现与相邻节段相似的退变表现,认为融合前椎间盘退变的自然史可能比融合本身的影响更明显[20]。因此椎间融合是否可引起相邻节段的退变一直是脊柱外科领域内富有争议的课题。通过建立椎间融合的动物模型进一步验证椎间融合是否能够加重相邻节段椎间盘退变成为必须。
在建立椎间盘退变动物模型的动物选择上,近15年来人们更倾向于较大的动物,如猴、猪、犬等哺乳动物[21]。理想的动物模型应能模仿人类的特定情节,这就要求动物模型在解剖和方法学上必须与临床相似,椎间融合只能在大型动物上进行,因为只有大型动物才有宽大的、平行的终板能进行椎间融合操作。一般来说,理想的椎间盘退变动物模型应具备以下条件[22]:与人椎间盘自然退变过程相似,能再现椎间盘退行性变的自然规律;模型重复性好;方法可行且经济效益良好。
实验选择比格犬作为模型动物,首先,因为其椎间盘解剖结构和生化成分与人类椎间盘接近,都属于软骨营养障碍型椎间盘;其次,相比于大鼠等小型动物来说,犬椎间盘具有宽大、平行的终板,方便实行椎间融合操作,而且更利于获取椎间盘组织,犬对手术创伤耐受能力更强。另外,犬虽为四肢动物,但喜好蹲坐,与人类腰椎间盘所处的生物力学环境接近,而且椎间融合要求在大型动物上进行,因此,实验使用比格犬作为椎间盘退变动物较实用、可行。
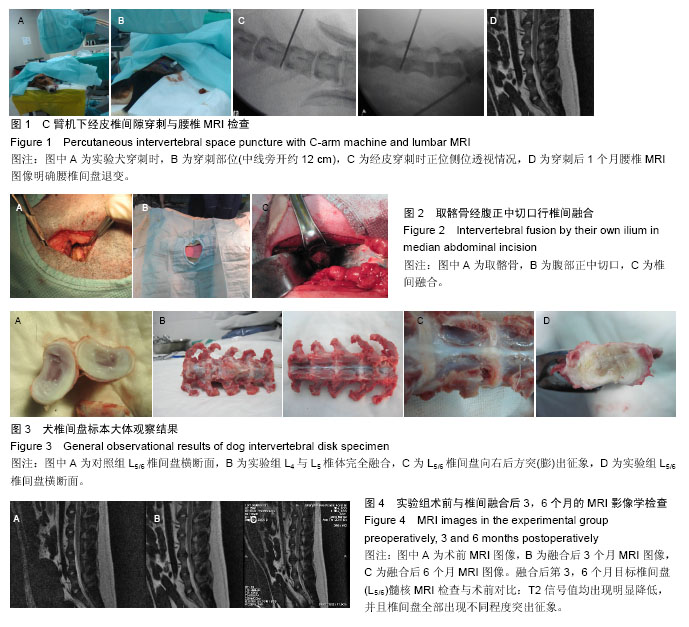
犬的脊柱解剖情况:犬脊柱主要由4大部分组成,颈椎、胸椎、腰椎和荐椎。犬有7枚颈椎、13枚胸椎、7枚腰椎和3枚荐椎,还有数量不一的尾骨或尾椎。椎间盘起始于第2和第3颈椎之间,终止于第7腰椎和第1荐椎之间。3枚荐椎融合在一起,类似于人类的骶骨。此次实验节段选择在L5/6间隙,融合节段选择在L4/5间隙。通过术后观察及比较两组L5/6椎间盘退变的程度来了解椎间融合后相邻节段退变程度与自然退变过程的区别。
犬腰椎间融合式主要有2种,前方经腹入路方式及侧前方经腹膜外入路方式。黄丽洁等[23]通过对比性研究发现侧前方腹膜后入路进行犬腰椎椎间融合的优点是不经腹腔操作,术后恢复快。但是该入路手术视野显露不够充分,而且椎体侧方肌肉发达,导致手术操作困难。同时狗的后腹膜非常菲薄,而且与周围组织紧密贴附,分离时容易导致后腹膜破裂,手术难度较大,手术操作时间长,手术出血多。而前方经腹入路方式是需要经腹腔操作,对实验动物腹部脏器影响比较大,容易引起肠粘连等并发症,不利于术后恢复。但该术式手术视野清晰,方便手术操作。
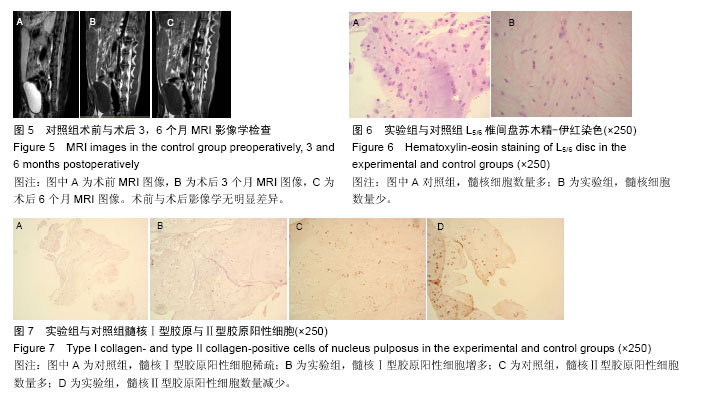
实验采用前方经腹入路方式,但术中并未切开前后腹膜,而是在腹直肌外侧缘将腹膜钝性分离,将腹膜腔推向对侧,分离至椎体前缘,避开腹主动脉,骨膜剥离器钝性分离椎体与周围组织,有小出血点电刀烧灼止血,确认L4,5椎间盘后,用尖刀将外层纤维环切开,用枪钳及髓核钳将椎间盘取出,并用刮勺将上下椎体终板刮除,置入取下的髂骨行椎间融合,该方法能不经过腹膜腔,对腹内脏器影响比较小,术后实验动物恢复较快,同时出血较少,术野清晰,但犬的腹膜非常薄,与周围组织贴附紧密,推开时容易破裂,实验组共有2只犬在行前路椎间融合时腹膜破裂,用可吸收线进行紧密缝合。但该术式仍然比经腹腔入路操作方便,术中少了腹内脏器的影响,术野清晰,操作时间更短。
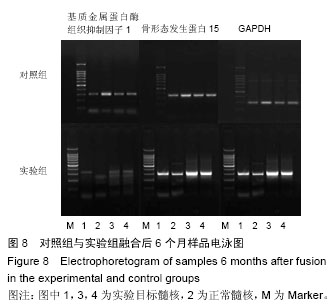
MRI检查对于腰椎间盘退变程度的评估较X射线、CT扫描等其他检查手段有以下独特的优点:能反映组织多个参数,可获得较CT更多信息;可直接进行矢状位、冠状位及水平位多平面图像扫描;椎间盘个部分包括纤维环、髓核和软骨终板在MRI图像上清晰可辨;具有极高的软组织分辨力,无骨伪影和发射损伤,可早期客观反映椎间盘退变情况[24]。Chatani等[25]在1993年报道了在椎间盘组织水含量超过75%时,MRI T2信号强度与含水量呈正相关,随着椎间盘含水量减少,MRI T2信号强度逐渐减低,在椎间盘组织含水量小于75%时,MRI T2信号强度与含水量之间无明显关联。这一研究结果说明,MRI T2加权像低信号反映出椎间盘开始丢失水分,由于这一征象比形态结构异常征象出现的要早,因此对椎间盘退变的早期诊断具有重要的临床价值。目前MRI评价腰椎间盘髓核退变程度,绝大多数为主观指标。Videman等[14]对髓核退变进行了半定量分析。根据髓核前中后3个部位分数之和算出退变分数,0分无退变,9分最严重。同时还以相邻脑脊液信号为参考标准,以髓核与脑脊液信号强度比值作为校正值,根据退变分数来定量分析退变程度,对于椎间盘退变程度特别是早期退变能够提供更准确的信息。Videman法是目前评价腰椎间盘髓核退变的较好方法。此次试验评估即使用该方法。
根据Videman法评估结果结合统计学方差分析结果提示,2组在融合3个月内椎间盘退变程度不相同,实验组明显快于对照组,随着时间的延长,实验组椎间盘退变程度较对照组更明显。椎间融合加剧相邻节段椎间盘退变,退变程度随时间延长而加重。
椎间盘退变后,其形态结构和生物化学组成都会发生明显改变,苏木精-伊红染色发现Ⅰ型胶原和Ⅱ型胶原的变化与椎间盘退变关系最为密切,其胶原含量占椎间盘总胶原含量的80%。Ⅰ型胶原主要存在于纤维环外层,Ⅱ型胶原主要存在于髓核内,它们分别在维持椎间盘张力和承受压力方面起着重要作用。在腰椎退变早期,髓核中Ⅱ型胶原含量即出现减少,而Ⅰ型胶原含量增加,这种趋势与椎间盘退变严重程度呈正比。在腰椎退变早期,髓核中的Ⅱ型胶原含量即出现减少,而Ⅰ型胶原增加,这种趋势与椎间盘退变严重程度成正比。因此,实验采用测量髓核中Ⅱ型胶原阳性细胞的变化来判断椎间盘的退变与否及程度。实验组融合第3,6个月髓核Ⅱ型胶原阳性细胞含量较对照组均明显减少,说明椎间融合后能引起相临节段椎间盘的退变的加重。实验组融合第6个月时目标节段L5/6髓核Ⅱ型胶原阳性细胞含量对比融合第3个月时减少,说明椎间融合后相邻节段椎间盘退变是持续进展的。
椎间盘内的蛋白多糖对水能产生很高的亲和力,对维持椎间盘内的水分含量具有重要作用,蛋白多糖能够与透明质酸形成聚合体,该聚合体对维持椎间盘的弹性具有重要作用。随之年龄的增长,椎间盘内水分丢失,蛋白多糖含量减少,蛋白多糖与透明质酸形成的聚合体也明显减少,椎间盘弹性减低,进一步影响了椎间盘的生理功能。蛋白多糖含量多少与椎间盘退变程度呈负相关,即蛋白多糖含量高椎间盘退变程度低,蛋白多糖含量低,间盘退变程度高,导致蛋白多糖减少的主要原因有:退变的椎间盘细胞合成蛋白多糖减少,蛋白多糖被基质金属蛋白酶降解为短肽片段。大量证据表明,椎间盘退变时基质金属蛋白酶含量明显高于正常水平,基质金属蛋白酶在基质下调过程中发挥着关键性作用,它与基质金属蛋白酶抑制剂的生成和相互作用的紊乱导致了椎间盘的退变。
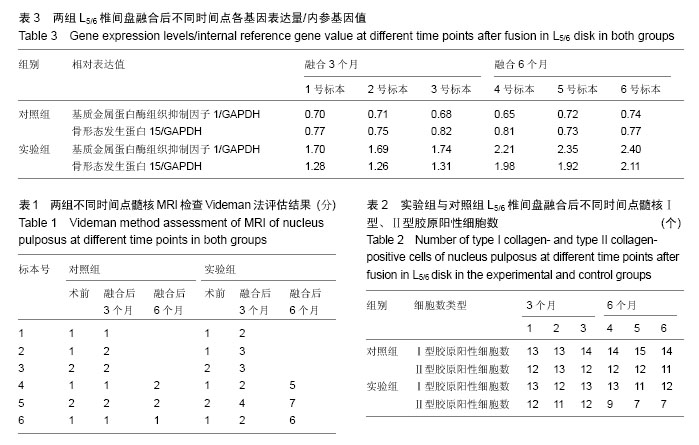
目前已发现3种基质金属蛋白酶组织抑制因子,基质金属蛋白酶组织抑制因子1、基质金属蛋白酶组织抑制因子2和基质金属蛋白酶组织抑制因子3。在退变椎间盘中可见基质金属蛋白酶组织抑制因子1和基质金属蛋白酶组织抑制因子2的表达,而基质金属蛋白酶组织抑制因子3的表达未见明显增加。Wallach 等从椎间盘退变疾病患者手术摘除的退变椎间盘中分离出髓核细胞,进行单纯培养后,用携带基质金属蛋白酶组织抑制因子1的腺病毒转染髓核细胞后,将该细胞在器皿中培养,进行蛋白多糖检测,最后发现细胞外基质中蛋白多糖合成明显增加,该实验认为基质金属蛋白酶组织抑制因子1可作为基因治疗椎间盘退行性疾病的一种有效的潜在的方法。因此,实验选择了基质金属蛋白酶组织抑制因子1为观察指标。
骨形态发生蛋白也是生长因子中的一种。有学者用含有骨形态发生蛋白的腺病毒转染人髓核细胞后,发现携带有多种骨形态发生蛋白的髓核细胞蛋白多糖表达都明显增多,且髓核细胞内胶原表达也明显增多,其中含有骨形态发生蛋白15,14的髓核细胞中蛋白多糖及胶原的表达增加最为显著,分别增加了552%、661%,因此实验选择骨形态发生蛋白15作为观察指标。
根据实验结果,知道椎间融合后相邻节段的椎间盘,在融合后3,6个月基质金属蛋白酶组织抑制因子1、骨形态发生蛋白15的相对表达量均明显增加,符合椎间盘退变后基因表达的改变;同时基质金属蛋白酶组织抑制因子1、骨形态发生蛋白15的表达与椎间盘退变程度具有正相关关系,因此,根据两组融合后3,6个月时基质金属蛋白酶组织抑制因子1、骨形态发生蛋白15表达量均呈现逐步增加趋势;对照组增加趋势没实验组明显。因此,得出结论:椎间融合引起相邻节段退变的动物实验模型的建立成功,椎间融合能加重相邻节段椎间盘退变,退变与时间呈正相关。
实验验证了腰椎融合能够引起相邻节段椎间盘退变加重,退变程度与时间呈正相关,椎间盘退变的动物模型建立成功,该实验有很好的可重复性,经济效益良好,同时该模型还可继续应用来检验脊柱非融合技术,用来验证脊椎非融合技术是否比脊柱融合更有优势,是否可减轻相邻节段椎间盘退变的发生。
.jpg)
.jpg)