中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (17): 2488-2495.doi: 10.3969/j.issn.2095-4344.2016.17.008
• 脊柱植入物 spinal implant • 上一篇 下一篇
椎弓根置钉修复胸腰椎骨折合并脊髓损伤:选择性损伤节段及全部固定节段植骨融合的比较
史晓林1,张 昊1,刘 磊1,史晓东2,金晓宁1,刘清阁1,袁伟东1
- 1保定市第二医院骨科,河北省保定市 071000;2保定德润医院,河北省保定市 071000
Pedicle screw fixation for thoracolumbar fracture with spinal cord injury: a comparison of the selective injury segment and the whole bone graft fusion
Shi Xiao-lin1, Zhang Hao1, Liu Lei1, Shi Xiao-dong2, Jin Xiao-ning1, Liu Qing-ge1, Yuan Wei-dong1
- 1Department of Orthopedics, the Second Hospital of Baoding City, Baoding 071000, Hebei Province, China; 2Derun Hospital, Baoding 071000, Hebei Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
运动节段:两个相邻的椎体、椎间盘、前后纵韧带、椎弓根、椎间关节、黄韧带、横突、棘突、棘间韧带、棘上韧带等组成脊柱单一运动节段。运动节段是脊柱的最小运动功能单元。运动节段被固定融合后,相应的应力集中到相邻的运动节段,可出现邻近节段椎间盘退行性改变、椎间不稳定、关节突间关节退变等。
损伤节段植骨融合:脊柱后路椎弓根内固定系统提供了坚强固定的同时,每增加一个融合节段,脊柱将损失5%的柔韧性。对脊柱单一运动单元选择性损伤节段植骨融合,可减少融合脊柱运动节段,保留运动单元功能,还可减少内固定失效,降低后凸畸形发生,同时还能够预防下腰痛发生。
背景:胸腰椎爆裂性骨折合并脊髓神经损伤在后路椎弓根螺钉内固定同时需进行椎管减压,脊柱后侧结构受到破坏,目前后外侧植骨融合所有固定节段仍然是主要的修复方法。为了进一步减少融合节段,保留运动单元,有必要在内固定及减压同时进行脊柱选择性融合。
目的:通过与后外侧全部固定节段植骨融合相比,探讨后外侧选择性损伤节段融合修复胸腰椎骨折合并脊髓神经损伤的优势。
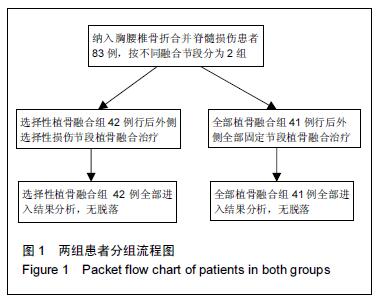
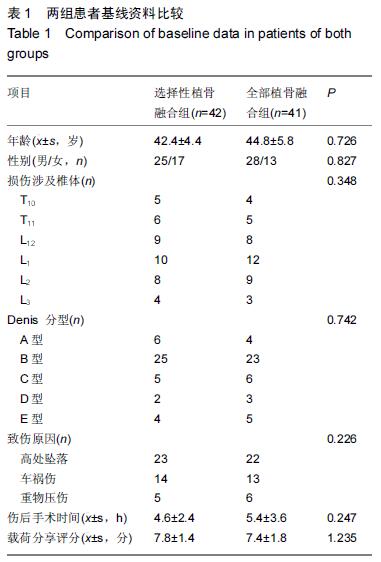
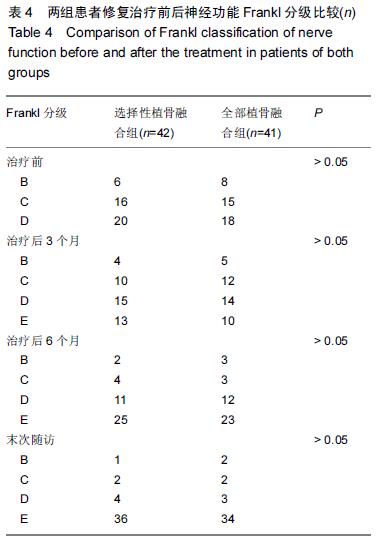
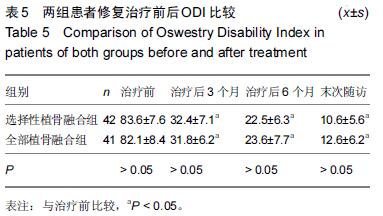
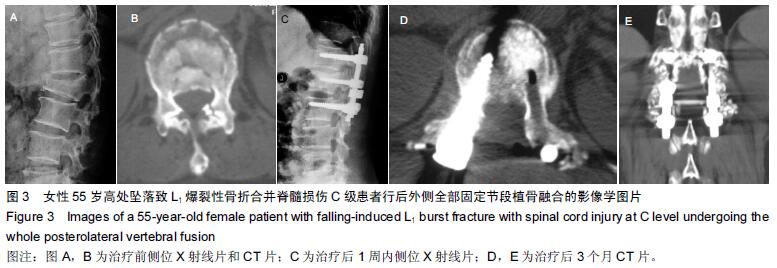
方法:对2006年1月至2013年7月采用后路短节段经伤椎单侧椎弓根置钉椎管减压、后外侧植骨融合修复胸腰椎爆裂骨折的83例患者资料进行回顾性分析,根据融合节段分组,选择性植骨融合组42例行后外侧选择性损伤节段植骨融合,全部植骨融合组41例行后外侧全部固定节段植骨融合。对两组患者的围手术期指标、内固定情况、伤椎椎体前缘高度丢失率、Cobb角、脊髓神经恢复及Oswestry功能障碍指数进行比较。
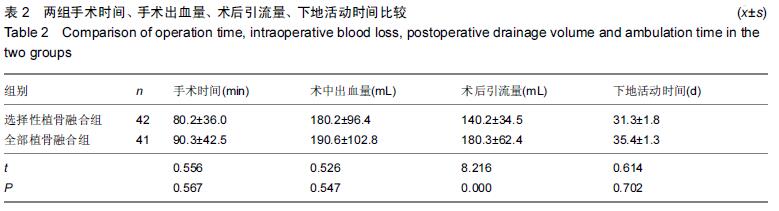
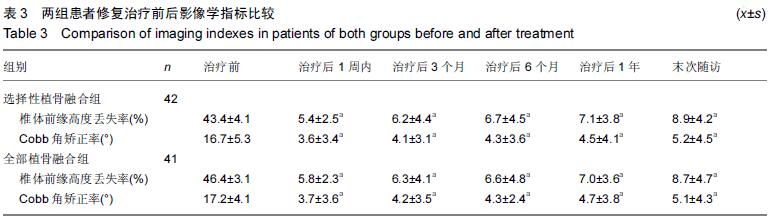
结果与结论:①所有患者均获得25-32个月随访。②两组患者手术时间、术中出血量及下地活动时间差异无显著性意义(P > 0.05);选择性植骨融合组术后引流量小于全部植骨融合组(P < 0.05)。两组患者取出内固定前无内固定松动及钉、棒断裂。③两组治疗后各时间点的伤椎椎体前缘高度丢失率、Cobb角与治疗前比较均明显改善(P < 0.05),两组间治疗后各时间点的伤椎椎体前缘高度丢失率、Cobb角差异无显著性意义(P > 0.05)。④两组间比较治疗后6个月完全融合率差异无显著性意义(P > 0.05);两组部分融合病例在内固定取出前全部融合。⑤两组治疗后脊髓神经功能均有一定程度恢复,末次随访Oswestry功能障碍指数两组间差异无显著性意义(P > 0.05)。⑥结果表明与后外侧全部固定节段植骨融合相比,后外侧选择性损伤节段植骨融合同样可以维持椎体高度及预防Cobb角再丢失,减少内固定松动、断裂。同时选择性损伤节段植骨融合在内固定取出后可减少脊柱运动单元丧失,从而降低邻近节段间盘退变发生。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0003-3878-3779(史晓林)

.jpg)