| [1] 李明豹,卢旭华.脊柱外科手术并发脑脊液漏的相关因素分析及防治措施[J].脊柱外科杂志,2009,6(7):368-369.
[2] Davis RA.A long-term outcome analysis of 984 surgically treated herniated lumbar discs.Neurosurg. 1994;80(3): 415-421.
[3] Waisman M, Schweppe Y.Postoperative cerebrospinal fluid leakage after lumbar spine operations. Conservative treatment.Spine (Phila Pa 1976). 1991;16(1):52-53.
[4] Hughes SA, Ozgur BM, German M, et al.Prolonged Jackson-Pratt drainage in the management of lumbar cerebrospinal fluid leaks.Surg Neurol. 2006; 65(4):410-414, discussion 414-415.
[5] 于滨生,郑召民,庄新明,等.脊柱手术后脑脊液漏的治疗[J].中国脊柱脊髓杂志,2009,19(2):113-116.
[6] 凌云,朱志华.脊柱手术并发脑脊液漏37例治疗体会[J].颈腰痛杂志,2012,33(5):355-356.
[7] Dafford EE, Anderson PA.Comparison of dural repair techniques.Spine J. 2015;15(5):1099-1105.
[8] Ghobrial GM, Maulucci CM, Viereck MJ,et al.Suture Choice in Lumbar Dural Closure Contributes to Variation in Leak Pressures: Experimental Model.J Spinal Disord Tech. 2014 Sep 8. [Epub ahead of print]
[9] Cain JE Jr, Rosenthal HG, Broom MJ, et al.Quantification of leakage pressures after durotomy repairs in the canine.Spine (Phila Pa 1976). 1990;15(9):969-970.
[10] Yu F, Wu F, Zhou R,et al.Current developments in dural repair: a focused review on new methods and materials.Front Biosci (Landmark Ed). 2013;18:1335-1343.
[11] Sekhar LN, Mai JC.Dural repair after craniotomy and the use of dural substitutes and dural sealants.World Neurosurg. 2013; 79(3-4):440-442.
[12] Epstein NE.Dural repair with four spinal sealants: focused review of the manufacturers' inserts and the current literature. Spine J. 2010; 10(12):1065-1068.
[13] Jankowitz BT, Atteberry DS, Gerszten PC, et al.Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009; 18(8):1169-1174.
[14] Epstein NE.Dural repair with four spinal sealants: focused review of the manufacturers' inserts and the current literature. Spine J. 2010; 10(12):1065-108.
[15] Miscusi M, Polli FM, Forcato S, et al.The use of surgical sealants in the repair of dural tears during non-instrumented spinal surgery.Eur Spine J. 2014;23(8):1761-1766.
[16] Hida K, Yamaguchi S, Seki T,et al.Nonsuture dural repair using polyglycolic acid mesh and fibrin glue: clinical application to spinal surgery.Surg Neurol. 2006; 65(2): 136-142; discussion 142-143.
[17] Shimada Y, Hongo M, Miyakoshi N, et al.Dural substitute with polyglycolic acid mesh and fibrin glue for dural repair: technical note and preliminary results.J Orthop Sci. 2006; 11(5):454-458.
[18] Kitchel SH, Eismont FJ, Green BA.Closed subarachnoid drainage for management of cerebrospinal fluid leakage after an operation on the spine.J Bone Joint Surg Am. 1989;71(7): 984-987.
[19] Guerin P, El Fegoun AB, Obeid I, et al.Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review.Injury. 2012; 43(4): 397-401.
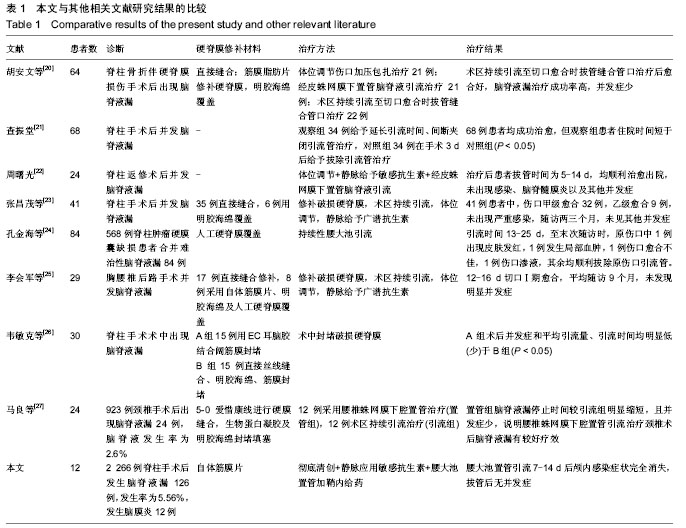
[20] 胡安文,李锋,蒲丹,等.不同方法治疗脊柱骨折伴硬脊膜损伤术后脑脊液漏的疗效比较[J].中华创伤杂志,2015,31(1):26-30.
[21] 查振堂.脊柱手术并发脑脊液漏的治疗体会[J].医药前沿,2015, (11):166-167.
[22] 周曙光.脊柱返修手术并发脑脊液漏的临床治疗措施[J].中外健康文摘,2014,(20):125-126.
[23] 张昌茂,陈祖星,刘国铭.41例脊柱手术后脑脊液漏的治疗[J].医药前沿,2014,(2):185-185.
[24] 孔金海,肖辉,孙正望,等.腰大池引流术在难治性脑脊液漏中的运用价值[J].脊柱外科杂志,2014,12(5):309-312.
[25] 李会军,苏巍,姚栋,等.胸腰椎后路手术并发脑脊液漏29例治疗体会[J].山西医药杂志,2014,43(15):1831-1833.
[26] 韦敏克,尹东,梁斌,等.脊柱手术术中脑脊液漏不同处理方法的疗效比较[J].中国临床新医学,2013,6(12):1147-1150.
[27] 马良,盛伟斌,邓强. 颈椎术后脑脊液漏治疗:不同引流方法比较[J].中国组织工程研究,2013,18(48):8413-8418.
[28] 于凤宾.应用复合PLGA纳米纤维膜构建人工硬脊膜修复羊硬脊膜缺损的实验研究[D].第二军医大学.2013.
[29] Eldrige JS,Weingarten TN,Rho RH. Management of cerebral spinal fluid leak complicating spinal cord stimulator implantation. Pain Pract. 2006;6(4):285-288.
[30] Maher CO, Meyer FB, Mokri B.Surgical treatment of spontaneous spinal cerebrospinal fluid leaks.Neurosurg Focus. 2000; 9(1):e7.
[31] 李霞.腰大池脑脊液持续外引流加鞘内注射治疗术后颅内感染疗效分析[J].中华实用诊断余治疗杂志,2009,24(5):481-482.
[32] Glassman SD, Dimar JR, Puno RM,et al.Salvage of instrumental lumbar fusions complicated by surgical wound infection.Spine (Phila Pa 1976). 1996;21(18):2163-2169.
[33] Mehbod AA, Ogilvie JW, Pinto MR, et al.Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure.J Spinal Disord Tech. 2005; 18(1):14-17.
[34] Richards BS.Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis.J Bone Joint Surg Am. 1995;77(4):524-529. |