[1] KORTHAUS A, KRAUSE M, PAGENSTERT G, et al. Tibial slope in the posterolateral quadrant with and without ACL injury. Arch Orthop Trauma Surg. 2021. doi: 10.1007/s00402-021-04298-w.
[2] LUCZKIEWICZ P, DASZKIEWICZ K, WITKOWSKI W, et al. Influence of meniscus shape in the cross sectional plane on the knee contact mechanics. J Biomech. 2015;48(8):1356-1363.
[3] SONG GY, LIU X, ZHANG H, et al. Increased Medial Meniscal Slope Is Associated With Greater Risk of Ramp Lesion in Noncontact Anterior Cruciate Ligament Injury. Am J Sports Med. 2016;44(8):2039-2046.
[4] 岳德波,鄂森,王佰亮,等.胫骨后倾与非接触性前交叉韧带断裂的关系及其对关节稳定性的影响[J].中华医学杂志,2013,93(17): 1309-1312.
[5] KUMAR PANIGRAHI T, DAS A, MOHANTY T, et al. Study of relationship of posterior tibial slope in anterior cruciate ligament injury. J Orthop. 2020;21:487-490.
[6] ALICI T, ESENYEL CZ, ESENYEL M, et al. Relationship between meniscal tears and tibial slope on the tibial plateau. Eurasian J Med. 2011;43(3): 146-151.
[7] WU J, HUANG JM, ZHAO B, et al. Risk Factors Comparison for Radial and Horizontal Tears. J Knee Surg. 2016;29(8):679-683.
[8] JIANG J, LIU Z, WANG X, et al. Increased Posterior Tibial Slope and Meniscal Slope Could Be Risk Factors for Meniscal Injuries: A Systematic Review. Arthroscopy. 2022;38(7):2331-2341.
[9] BERNHOLT D, DEPHILLIPO NN, AMAN ZS, et al. Increased posterior tibial slope results in increased incidence of posterior lateral meniscal root tears in ACL reconstruction patients. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3883-3891.
[10] HASHEMI J, CHANDRASHEKAR N, MANSOURI H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1): 54-62.
[11] OKAZAKI Y, FURUMATSU T, KODAMA Y, et al. Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29(1):44-50.
[12] KHAN N, MCMAHON PANDOBAID H. Bony morphology of the knee and non-traumatic meniscal tears: is there a role for meniscal impingement? Skeletal Radiol. 2014;43(7):955-962.
[13] MOON HS, CHOI CH, JUNG M, et al. Medial Meniscal Posterior Horn Tears Are Associated With Increased Posterior Tibial Slope: A Case-Control Study. Am J Sports Med. 2020;48(7):1702-1710.
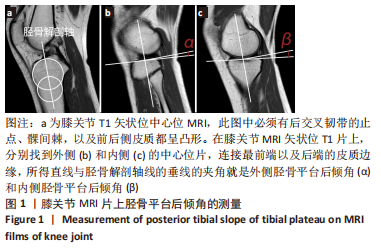
[14] HUDEK R, SCHMUTZ S, REGENFELDER F, et al. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066-2072.
[15] HASHEMI J, CHANDRASHEKAR N, GILL B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724-2734.
[16] BERNHARDSON AS, AMAN ZS, DEPHILLIPO NN, et al. Tibial Slope and Its Effect on Graft Force in Posterior Cruciate Ligament Reconstructions. Am J Sports Med. 2019;47(5):1168-1174.
[17] DE BOER JJ, BLANKEVOORT L, KINGMA I, et al. In vitro study of inter-individual variation in posterior slope in the knee joint. Clin Biomech (Bristol, Avon). 2009;24(6):488-492.
[18] QI Y, SUN H, FAN Y, et al. Three dimensional finite element analysis of the influence of posterior tibial slope on the anterior cruciate ligament and knee joint forward stability. J Back Musculoskelet Rehabil. 2018;31(4):629-636.
[19] JOJIMA H, WHITESIDE LAANDOGATA K. Effect of tibial slope or posterior cruciate ligament release on knee kinematics. Clin Orthop Relat Res. 2004;(426):194-198.
[20] JENNY JY, BOÉRI C, BALLONZOLI L, et al. Difficultés et reproductibilité de la mesure radiographique de l’axe épiphysaire proximal du tibia selon la technique de Lévigne. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(7):658-663.
[21] Zhang Y, Chen Y, Qiang M,et al. Comparison between three-dimensional CT and conventional radiography in proximal tibia morphology. Medicine (Baltimore). 2018;97(30):e11632.
[22] Waiwaiole A, Gurbani A, Motamedi K,et al. Relationship of ACL Injury and Posterior Tibial Slope With Patient Age, Sex, and Race. Orthop J Sports Med. 2016;4(11):2325967116672852.
[23] HOHMANN E, TETSWORTH K, GLATT V, et al. Medial and Lateral Posterior Tibial Slope Are Independent Risk Factors for Noncontact ACL Injury in Both Men and Women. Orthop J Sports Med. 2021;9(8): 23259671211015940.
[24] 孙英华.年龄相关的胫骨平台后倾角变化规律与交叉韧带损伤关系的临床研究[D].济南:山东大学, 2016.
[25] WANG YL, YANG T, ZENG C, et al. Association Between Tibial Plateau Slopes and Anterior Cruciate Ligament Injury: A Meta-analysis. Arthroscopy. 2017;33(6):1248-1259.e4.
[26] CHURCH S, KEATING JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87(12):1639-1642.
[27] KOLBE R, SCHMIDT-HEBBEL A, FORKEL P, et al. Steep lateral tibial slope and lateral-to-medial slope asymmetry are risk factors for concomitant posterolateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2585-2591.
[28] THORLUND JB, JUHL CB, INGELSRUD LH, et al. Risk factors, diagnosis and non-surgical treatment for meniscal tears: evidence and recommendations: a statement paper commissioned by the Danish Society of Sports Physical Therapy (DSSF). Br J Sports Med. 2018;52(9): 557-565.
[29] FEUCHT MJ, BIGDON S, BODE G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34.
[30] MARKL I, ZANTOP T, ZEMAN F, et al. The effect of tibial slope in acute ACL-insufficient patients on concurrent meniscal tears. Arch Orthop Trauma Surg. 2015;135(8):1141-1149.
[31] BALCAREK P, TERWEY A, JUNG K, et al. Influence of tibial slope asymmetry on femoral rotation in patients with lateral patellar instability. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2155-2163.
[32] SONG GY, ZHANG H, ZHANG J, et al. Greater Static Anterior Tibial Subluxation of the Lateral Compartment After an Acute Anterior Cruciate Ligament Injury Is Associated With an Increased Posterior Tibial Slope. Am J Sports Med. 2018;46(7):1617-1623.
[33] MINAMI T, MUNETA T, SEKIYA I, et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1174-1181.
[34] 张艺, 亓建洪.胫骨平台后倾角与半月板损伤的相关性研究进展[J].中国矫形外科杂志,2020,28(8):721-724.
[35] GIFFIN JR, VOGRIN TM, ZANTOP T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376-382.
[36] CHOI CJ, CHOI YJ, SONG IB, et al. Characteristics of radial tears in the posterior horn of the medial meniscus compared to horizontal tears. Clin Orthop Surg. 2011;3(2):128-132. |