中国组织工程研究 ›› 2023, Vol. 27 ›› Issue (18): 2903-2909.doi: 10.12307/2023.308
• 骨与关节图像与影像 bone and joint imaging • 上一篇 下一篇
老年腰椎管狭窄症矢状位腰椎-骨盆序列的解析与重建
肖士鹏1,郭 辰2,李士春1,李钦亮1,许 勇1,徐 帅2
- 1北京市石景山医院骨科,北京市 100040;2北京大学人民医院脊柱外科,北京市 100044
Analysis and reconstruction of sagittal lumbo-pelvic parameters in the elderly with lumbar spinal stenosis
Xiao Shipeng1, Guo Chen2, Li Shichun1, Li Qinliang1, Xu Yong1, Xu Shuai2
- 1Department of Orthopedics, Beijing Shijingshan Hospital, Beijing 100040, China; 2Department of Spinal Surgery, Peking University People’s Hospital, Beijing 100044, China
摘要:
文题释义:
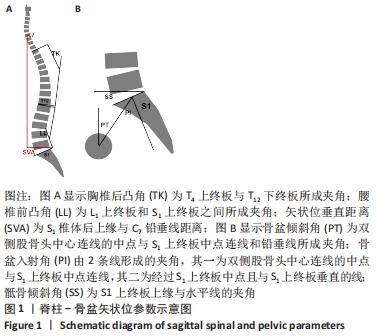
骨盆入射角:由2条线形成的夹角,其一为双侧股骨头中心连线的中点与S1上终板中点连线,其二为经过S1上终板中点且与S1上终板垂直的线。骨盆入射角是脊柱最重要的特征参数之一,一般在骨骼发育成熟后是固定不变的,在脊柱-骨盆矢状位参数的解析和构建中具有基石作用。
腰椎-骨盆匹配:最常用骨盆入射角减去腰椎前凸角、骨盆倾斜角表示,认为矢状面重建的目标是:骨盆倾斜角< 20°,腰椎前凸角=±9°,但是近年来研究发现这一重建目标存在诸多缺陷,未考虑年龄、性别、种族、体位、手术等影响因素,甚至骨盆入射角本身也非一成不变的,而这也是此次研究的意义所在。
背景:老年人群腰椎管狭窄症是脊柱最常见的退变性疾病,其症状和术后疗效与局部序列和整体平衡均相关,而关于该人群脊柱-骨盆矢状位参数的合理范围尚未可知。
目的:探究并验证腰椎管狭窄症患者手术前后腰椎-骨盆矢状位参数的匹配范围。
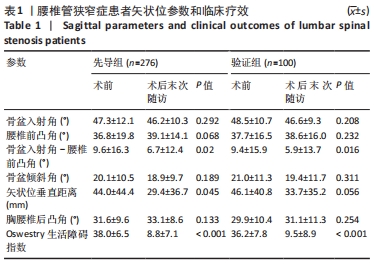
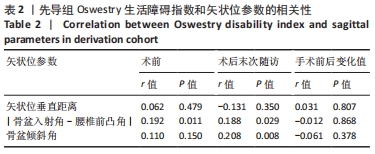
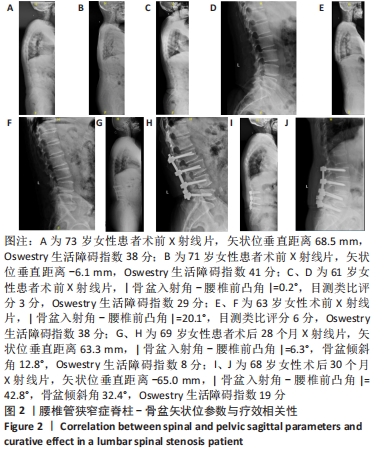
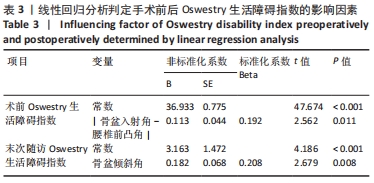
方法:选择2016年6月至2019年12月北京大学人民医院收治的腰椎管狭窄症患者376例,根据倾向性匹配评分原则,按照(2-3)∶1的配比分为先导组(n=276)与验证组(n=100),在术前与术后末次随访时进行影像学检查,获取脊柱-骨盆矢状位参数,包括胸椎后凸角、腰椎前凸角、骨盆入射角、骨盆倾斜角和矢状位垂直距离,上述参数在术前和末次随访时获得,其中|骨盆入射角-腰椎前凸角|、骨盆倾斜角和矢状位垂直距离为主要参数。以Oswestry生活障碍指数为生活质量评价指标,将手术前后Oswestry生活障碍指数取值范围分为轻度、较轻度、较重度、重度4个区间,手术前后Oswestry生活障碍指数所对应的矢状位参数合理阈值通过线性回归分析和Logistic回归进行双重判定。验证组主要对先导组结论进行验证。
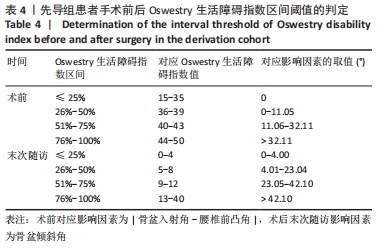
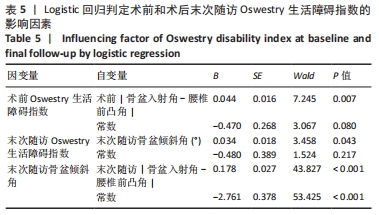
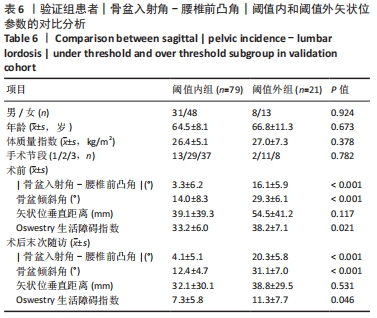
结果与结论:①先导组患者术后末次随访Oswestry生活障碍指数明显改善,术前Oswestry生活障碍指数与|骨盆入射角-腰椎前凸角|呈正相关(P=0.011),术后末次随访Oswestry生活障碍指数与|骨盆入射角-腰椎前凸角|和骨盆倾斜角呈正相关(P=0.029,P=0.008),与矢状位垂直距离无明确相关性。②先导组患者术前Oswestry生活障碍指数轻度、较轻度、较重度、重度对应的分值为15-35分、36-39分、40-43分、44-50分,术后末次随访轻度、较轻度、较重度、重度对应的分值为0-4分、5-8分、9-12分、13-40分。多元回归分析显示,术前Oswestry生活障碍指数的独立影响因素为|骨盆入射角-腰椎前凸角|,存在拟合公式Oswestry生活障碍指数=0.19×|骨盆入射角-腰椎前凸角|+36.9。通过双重判定,术前|骨盆入射角-腰椎前凸角|平均阈值为10.7°。术后Oswestry生活障碍指数的独立影响因素为骨盆倾斜角,骨盆倾斜角的独立影响因素为|骨盆入射角-腰椎前凸角|,存在公式Oswestry生活障碍指数=0.21×骨盆倾斜角+3.16和骨盆倾斜角=0.60×|骨盆入射角-腰椎前凸角|+12.22。③通过线性回归和logistic回归分析双重判定得出,术后|骨盆入射角-腰椎前凸角|的平均阈值为16.0°、骨盆倾斜角为23.1°。④验证组中,术后|骨盆入射角-腰椎前凸角|小于阈值的患者平均Oswestry生活障碍指数优于|骨盆入射角-腰椎前凸角超过阈值者|(P=0.046)。⑤|骨盆入射角-腰椎前凸角|=16.0°或许是针对老年腰椎管狭窄症后路手术矢状位参数的合理范围,提示针对该人群可适当放宽腰椎-骨盆的匹配程度。
https://orcid.org/0000-0003-1362-0025 (肖士鹏)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: