[1] ROYECA JM, CUNNINGHAM CM, PANDIT H, et al. Complex regional pain syndrome as a result of total knee arthroplasty: A case report and review of literature. Case Rep Womens Health. 2019;23:e00136.
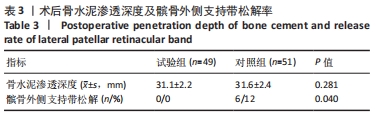
[2] LU C, SONG M, CHEN J, et al. Does tourniquet use affect the periprosthetic bone cement penetration in total knee arthroplasty? A meta-analysis. J Orthop Surg Res. 2020;15(1):602.
[3] CAWLEY DT, KELLY N, MCGARRY JP, et al. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J. 2013;95-b(3):295-300.
[4] HOFMANN AA, GOLDBERG TD, TANNER AM, et al. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty. 2006;21(3):353-357.
[5] ARTHUR JR, SPANGEHL MJ. Tourniquet Use in Total Knee Arthroplasty. J Knee Surg. 2019;32(8):719-729.
[6] AHMED I, CHAWLA A, UNDERWOOD M, et al. Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery. Bone Joint J. 2021;103-B(5):830-839.
[7] MAISTRELLI GL, ANTONELLI L, FORNASIER V, et al. Cement penetration with pulsed lavage versus syringe irrigation in total knee arthroplasty. Clin Orthop Relat Res. 1995;312:261-265.
[8] ARGENSON JN, PARRATTE S, ASHOUR A, et al. The outcome of rotating-platform total knee arthroplasty with cement at a minimum often years of follow-up. J Bone Joint Surg Am. 2012;94:638-644.
[9] FENG B, WENG X, LIN J, et al. Long-term follow-up of cemented fixed-bearing total knee arthroplasty in a Chinese population: a survival analysis of more than 10 years. J Arthroplasty. 2013;28:1701-1706.
[10] PETERS CL, CRAIG MA, MOHR RA, et al. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res. 2003;409:158-168.
[11] EWALD FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9-12.
[12] GOMES LS, BECHTOLD JE, GUSTILO RB. Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res. 1988;(236):72-81.
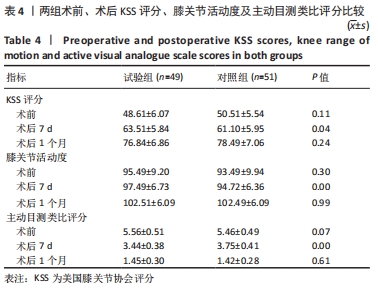
[13] DENNIS DA, KITTELSON AJ, YANG CC, et al. Does Tourniquet Use in TKA Affect Recovery of Lower Extremity Strength and Function? A Randomized Trial. Clin Orthop Relat Res. 2016;474(1):69-77.
[14] PARVIZI J, DIAZ-LEDEZMA C. Total knee replacement with the use ofa tourniquet: more pros than cons. Bone Joint J. 2013;95:133-134.
[15] CHEN S, LI J, PENG H, et al. The influence of a half-course tourniquet strategy on peri-operative blood loss and early functional recovery in primary total knee arthroplasty. Int Orthop. 2014;38:355-359.
[16] FENG L, ZHANG XG, YANG QG, et al. Effects of tourniquet on cardiac function in total knee arthroplasty with trans-esophageal echocardiography. Zhonghua Yi Xue Za Zhi.2013;93:3755-3757.
[17] ZHANG W, LI N, CHEN S, et al. The effects of a tourniquet used in total knee arthroplasty: a metaanalysis. J Orthop Surg Res. 2014;9:13.
[18] LEDIN H, ASPENBERG P, GOOD L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012;83:499-503.
[19] TAI TW, CHANG CW, LAI KA, et al. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2012; 94(24):2209-2215.
[20] LI B, WEN Y, WU H, et al. The effectof tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33(5):1263-1268.
[21] HARRIS LW, REID D, POWERS SK, et al. Tourniquet-induced skeletal muscle oxidative injury during lower limb orthopaedic trauma surgery. Bone Jt J. 2011;93:557.
[22] PFITZNER T, VON ROTH P, VOERKELIUS N, et al. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:96-101.
[23] BANWART JC, MCQUEEN DA, FRIIS EA, et al. Negative pressure intrusion cementing technique for total knee arthroplasty. J Arthroplasty. 2000; 15:360-367.
[24] JAWHAR A, STETZELBERGER V, KOLLOWA K, et al. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019; 27(7):2071-2081.
[25] MITTAL R, KO V, ADIE S, et al. Tourniquet application only during cement fxation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg. 2012;82:428-433.
[26] HASANAIN MS, APOSTU D, ALREFAEE A, et al. Comparing the effect of tourniquet vs tourniquet-less in simultaneousbilateral total knee arthroplasties. J Arthroplasty. 2018;33:2119-2124.
[27] KUMAR N, YADAV C, SINGH S, et al. Evaluation of pain in bilateral total knee replacement withand without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. 2015;6:85-88.
[28] EJAZ A, LAURSEN AC, KAPPEL A, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85:422-426.
[29] ALEXANDERSSON M, WANG EY, ERIKSSON S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the frst 3 months after surgery: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2019;27:1035-1042.
[30] HELLER S, CHEN A, RESTREPO C, et al. Tourniquet release prior to dressing application reduces blistering following total knee arthroplasty. J Arthroplasty.2015;30(7):1207-1210.
[31] KOMATSU T, ISHIBASHI Y, OTSUKA H, et al. The effect of surgicall approache sand tourniquet tapplication on patella femoral tracking in total knee arthroplasty. J Arthroplasty. 2003;18(3):308-312.
[32] VAISHYA R, AGARWAL AK, VIJAY V, et al. Short term outcomes of long duration versus short duration tourniquet in primary total knee arthroplasty: A randomized controlled trial. J Clin Orthop Trauma. 2018;9(1):46-50.
|