[1] SLOBOGEAN GP, SPRAGUE SA, SCOTT T, et al. Complications following young femoral neck fractures. Injury. 2015;46(3):484-491.
[2] LY TV, SWIONTKOWSKI MF. Treatment of Femoral Neck Fractures in Young Adults. J Bone Joint Surg Am. 2008;90A(10):2254-2266.
[3] UPADHYAY A, JAIN P, MISHRA P, et al. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86(7):1035-1040.
[4] DAVIDOVITCH RI, JORDAN CJ, EGOL KA, et al. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236-242.
[5] MIR H, COLLINGE C. Application of a medial buttress plate may prevent many treatment failures seen after fixation of vertical femoral neck fractures in young adults. Med Hypotheses. 2015;84(5):429-433.
[6] 李文龙, 梅沉成, 范亚楠, 等. 1/3管状板联合空心加压螺钉内固定术治疗青壮年 Pauwels Ⅱ、Ⅲ型股骨颈骨折43例[J]. 山东医药, 2016,56(27):92-94.
[7] PUTNAM SM, COLLINGE CA, GARDNER MJ, et al. Vascular Anatomy of the Medial Femoral Neck and Implications for Surface Plate Fixation. J Orthop Trauma. 2019;33(3):111-115.
[8] STACEY SC, RENNINGER CH, HAK D, et al. Tips and tricks for ORIF of displaced femoral neck fractures in the young adult patient. Eur J Orthop Surg Traumatol. 2016;26(4):355-363.
[9] WANG S, YANG J, SHEN H, et al. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury. 2015;46(10):1969-1974.
[10] GARDEN RS. Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br. 1971;53(2):183-197.
[11] MOLNAR RB, ROUTT MJ. Open reduction of intracapsular hip fractures using a modified Smith-Petersen surgical exposure. J Orthop Trauma. 2007;21(7):490-494.
[12] LUTTRELL K, BELTRAN M, COLLINGE CA. Preoperative decision making in the treatment of high-angle “vertical” femoral neck fractures in young adult patients. An expert opinion survey of the Orthopaedic Trauma Association’s (OTA) membership. J Orthop Trauma. 2014;28(9): e221-e225.
[13] STANNARD JP, HARRIS HW, VOLGAS DA, et al. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;(377):44-56.
[14] YE Y, HAO J, MAUFFREY C, et al. Optimizing Stability in Femoral Neck Fracture Fixation. Orthopedics. 2015;38(10):625-630.
[15] 杨义,于志亮,郭连霞,等.同种异体腓骨段联合加压空心钉内固定术治疗青壮年股骨颈移位骨折[J]. 中国医师杂志,2014(z1):119-120.
[16] KUNAPULI SC, SCHRAMSKI MJ, LEE AS, et al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma. 2015;29(3):144-150.
[17] GUMUSTAS SA, TOSUN HB, AGIR I, et al. Influence of number and orientation of screws on stability in the internal fixation of unstable femoral neck fractures. Acta Orthop Traumatol Turc. 2014;48(6):673-678.
[18] GIORDANO V, ALVES DD, PAES RP, et al. The role of the medial plate for Pauwels type III femoral neck fracture: a comparative mechanical study using two fixations with cannulated screws. J Exp Orthop. 2019;6(1):18.
[19] 周孝乾, 田智勇, 陈洪强, 等. 比基尼入路切开复位PFNA与闭合空心钉治疗青壮年股骨颈骨折的疗效比较[J]. 中华老年骨科与康复电子杂志,2020,6(5):251-256.
[20] 杨晓秋, 赵滨, 叶赟, 等. 切开复位PFNA内固定治疗青壮年移位型股骨颈骨折近期疗效观察[J]. 贵州医药,2018,42(8):998-999.
[21] ZLOWODZKI M, AYENI O, PETRISOR BA, et al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163-169.
[22] 丁强, 孙楠, 吴非燃, 等. 空心钉附加内侧支撑钢板内固定治疗青壮年非头下型股骨颈骨折的疗效观察[J]. 中国骨与关节损伤杂志, 2018,33(5):534-535.
[23] YE Y, CHEN K, TIAN K, et al. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury. 2017;48(10):2189-2193.
[24] ZHUANG L, WANG L, XU D, et al. Anteromedial femoral neck plate with cannulated screws for the treatment of irreducible displaced femoral neck fracture in young patients: a preliminary study. Eur J Trauma Emerg Surg. 2019;45(6):995-1002.
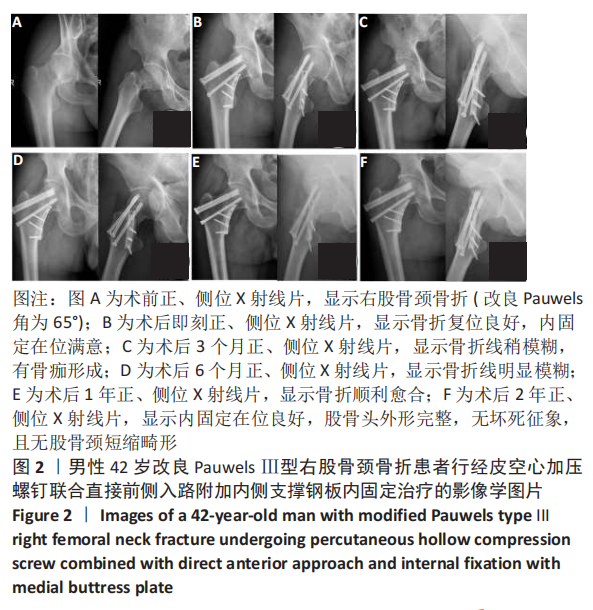
[25] 林绪超, 何文, 郑竑, 等. 经皮空心钉联合DAA入路微创支撑钢板内固定治疗青壮年Pauwels Ⅲ型股骨颈骨折的近期疗效[J]. 中国骨与关节损伤杂志,2019,34(6):593-595.
[26] MARCHAND LS, KARNS M, HIGGINS TF, et al. Femoral Neck Fracture Fixation with a Medial Buttress Plate That Led to Impingement with Hip Flexion: A Case Report. JBJS Case Connect. 2019;9(1):e21.
[27] ZLOWODZKI M, AYENI O, PETRISOR BA, et al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163-169.
[28] GAUTIER E, GANZ K, KRUGEL N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679-683.
[29] LAZARO LE, KLINGER CE, SCULCO PK, et al. The terminal branches of the medial femoral circumflex artery: the arterial supply of the femoral head. Bone Joint J. 2015;97-B(9):1204-1213.
[30] PAPAKOSTIDIS C, PANAGIOTOPOULOS A, PICCIOLI A, et al. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome.Injury. 2015;46(3):459-466.
[31] SLOBOGEAN GP, SPRAGUE SA, SCOTT T, et al. Management of young femoral neck fractures: is there a consensus? Injury. 2015;46(3):435-440.
|